I HAVE DENSE BREASTS…NOW WHAT?
- Ask for a 3D mammogram (digital breast tomosynthesis) if available (instead of a digital 2D mammogram).
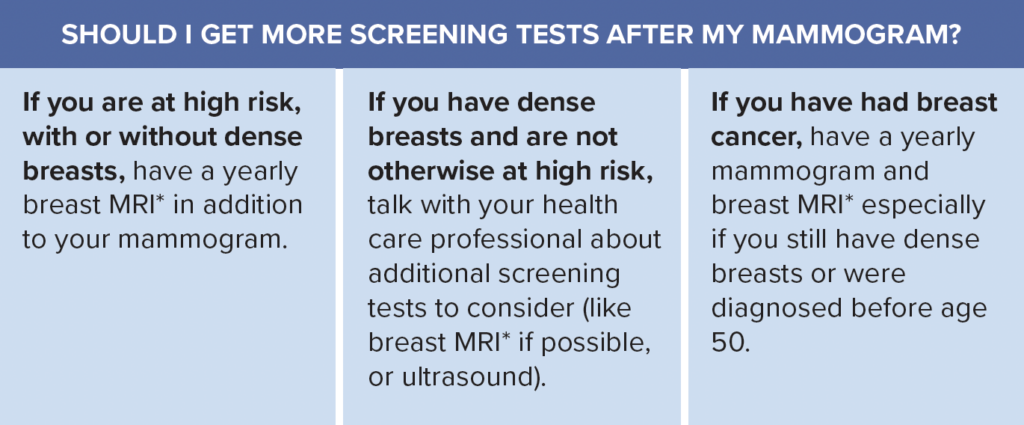
- Ask about additional screening tests that can find cancer that may be hidden on a mammogram.
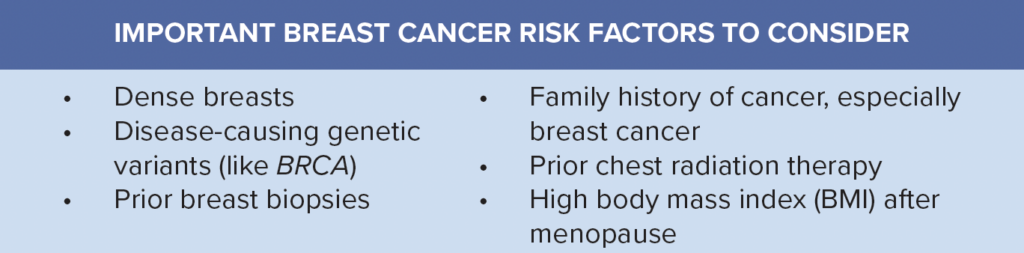
- The type of additional screening tests recommended will depend on your breast density and other risk factors. Talk with your health professional to learn your risk level and what tests may be right for you.
- You can do a risk assessment using free tools, such as: https://ibis.ikonopedia.com. If your lifetime risk of breast cancer is 20% or greater, you are “high risk.”
*If you are not able to have a breast MRI, a contrast-enhanced mammogram (CEM) or molecular breast imaging (MBI) are other options. Ultrasound can be considered if these options are not possible.
Europeans: The European Society of Breast Imaging recommends that women with extremely dense breasts aged 50 to 70 years be offered breast MRI every 2 to 4 years. If breast MRI is unavailable, ultrasound with mammography may be used.