NEWS: The FDA has issued a national requirement for dense breast reporting to patients and their referring providers, effective 09/10/2024. More here.
 Download Map Image (above) Download Insurance Map Image Download State Legislation Table
Download Map Image (above) Download Insurance Map Image Download State Legislation Table Notification Required by State
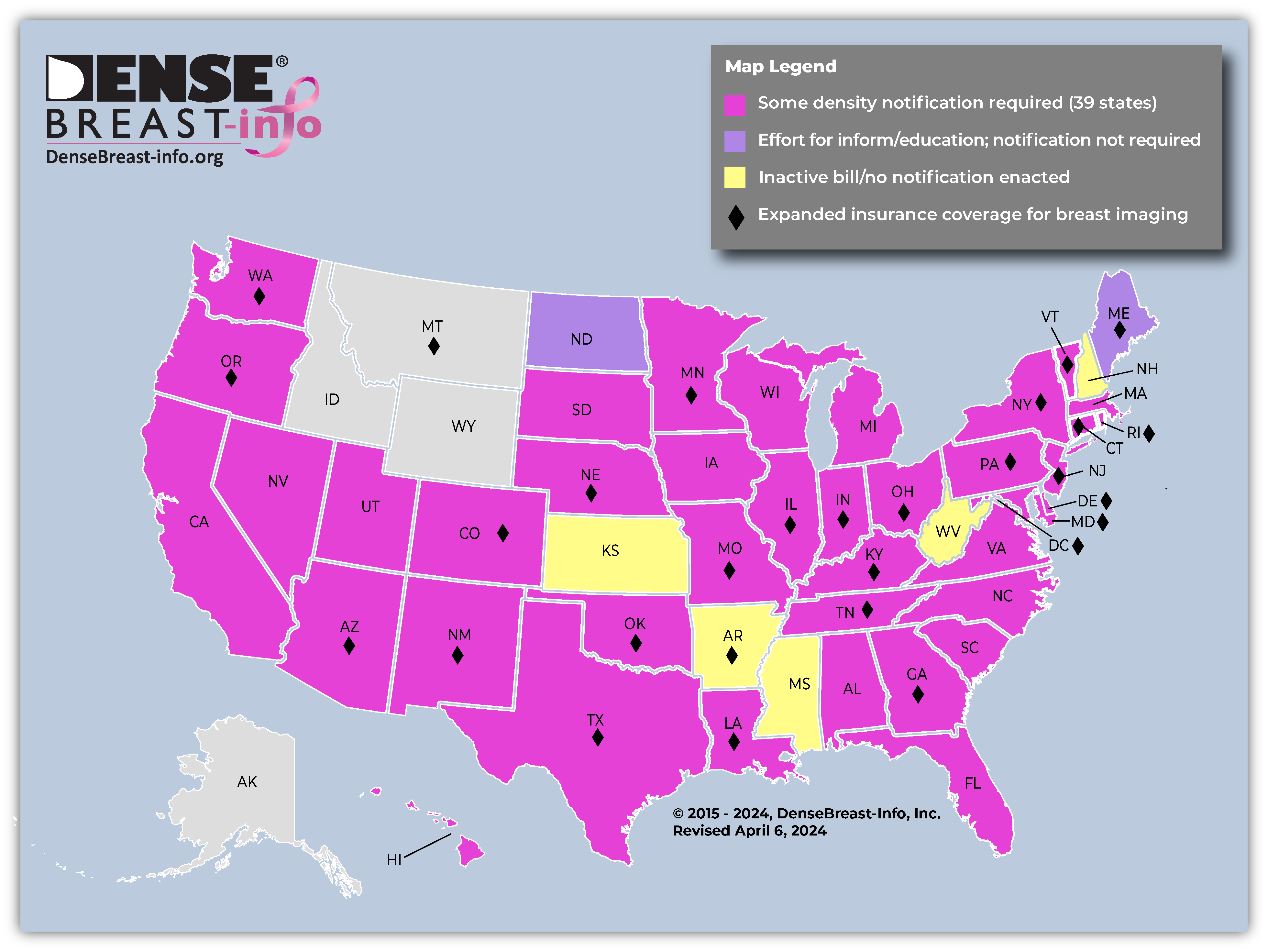
- Based on DBI analysis, currently 39 states and the District of Columbia require some level of breast density notification after a mammogram. Please note, not all laws require a patient be informed about her own breast density; some laws require only general notification about breast density.
- Though some state laws are more similar than others, there is no standard from state-to-state on what patients are told or how patients will be informed.
Insurance Coverage by State (denoted by a ◆ on the map)
- If there is a state insurance law, are all women covered? NO. A state insurance law does not necessarily apply to all policies within the state. For instance, self-funded plans, out-of-state plans, and national insurance plans (like Medicare) may be exempt from state laws.
- If there is no state insurance law, or if a plan is exempt from state law, might additional testing be covered? YES. While indicated states have some level of insurance coverage, generally, in other states, additional screening will be covered (subject to deductible/copay) if ordered by a physician.
- Patients should check with their insurance company regarding details of their coverage.
Federal Level
Alabama
Effective date: 8/1/2013
Who receives: Patient whose mammogram indicates heterogeneously or extremely dense breasts
How informed: In the letter sent to patients after their mammogram.
Notification required: “Your mammogram shows that your breast tissue is dense. Dense breast tissue is very common and is not abnormal. However, dense breast tissue may make it harder to find cancer on a mammogram and may also be associated with an increased risk of breast cancer. This information about the result of your mammogram is given to you to raise your awareness. Use this information to talk to your doctor about your own risks for breast cancer. At that time, ask your doctor if more screening tests might be useful, based on your risk. A report of your results was sent to your physician.”
Back To TopAlaska
No density notification or insurance legislation has been introduced.
Back To TopArizona
Effective date: 10/1/2014
Who receives: Patient whose mammogram indicates heterogeneously or extremely dense breasts.
How informed: In the letter sent to patients after their mammogram.
Notification required: “Your mammogram indicates that you have dense breast tissue. Dense breast tissue is common and is found in fifty percent of women. However, dense breast tissue can make it more difficult to detect cancers in the breast by mammography and may also be associated with an increased risk of breast cancer. This information is being provided to raise your awareness and to encourage you to discuss with your health care providers your dense breast tissue and other breast cancer risk factors. Together, you and your physician can decide if additional screening options are right for you. A report of your results was sent to your physician.”
Insurance, effective 90 days after regular 2023 session ends, “A contract that provides coverage for surgical services for a mastectomy shall also provide coverage for preventive mammography screening and diagnostic imaging performed on dedicated equipment for diagnostic purposes on referral by a patient’s physician, subject to all of the terms and conditions of the policy, including: Digital Breast Tomosynthesis, Magnetic Resonance Imaging, Ultrasound or other modality and at such age and intervals as recommended by the national comprehensive cancer network. This includes patients at risk for breast cancer who have a family history with one or more first or second degree relatives with breast cancer, prior diagnosis of breast cancer, positive testing for hereditary gene mutations or heterogeneously or dense breast tissue based on the breast imaging reporting and data system of the American College of Radiology.”
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To TopArkansas
A 2019 “inform” bill (HB 1473) was introduced but later withdrawn after the federal law ensuring development of a national reporting standard was signed.
Insurance amendment, effective 8/2021 (estimated):
All women: An insurance policy shall not impose a copayment or deductible for a screening mammogram, including digital breast tomosynthesis (3D mammography), or breast ultrasound
Insurance providers shall offer as an essential benefit: “Every health care insurer in this state shall offer, as an essential health benefit, coverage for screening mammography: (A) A baseline mammogram for an insured woman who is thirty-five to forty (35-40) years of age; (B) An annual mammogram for an insured woman who is forty (40) years of age or older; (C) Upon recommendation of a woman’s physician, without regard to age, when the woman has had a prior history of breast cancer, when the woman’s mother, or sister, or any first or second degree female relative of the woman has had a history of breast cancer, positive genetic testing, or other risk factors; and (D) complete breast ultrasound if a mammogram screening demonstrates heterogeneously dense or extremely dense breast tissue and the woman’s primary healthcare provider or radiologist determines an ultrasound screening is medically necessary.”
Insurance amendment, effective 8/2019 (estimated):
All women: An insurance policy shall not impose a copayment or deductible for a screening mammogram, including digital breast tomosynthesis (3D mammography).
Insurance providers shall offer as an essential benefit: “A comprehensive ultrasound screening of an entire breast or breasts if a mammogram screening demonstrates heterogeneously dense or extremely dense breast tissue and the woman’s primary healthcare provider or radiologist determines a comprehensive ultrasound screening is medically necessary.” “A breast ultrasound may be subject to any applicable copayment as required under a health benefit plan but shall not be subject to a deductible.”
“Insurance coverage for screening mammograms, including digital breast tomosynthesis (3D), and breast ultrasounds shall not prejudice coverage for diagnostic mammograms or breast ultrasounds as recommended by the woman’s physician.”
Insurance, effective 8/3/2017 (estimated):
All women: An insurance policy shall not impose a copayment or deductible for a screening mammogram, including digital breast tomosynthesis (3D mammography).
Insurance providers shall offer as an essential benefit: “A comprehensive ultrasound screening of an entire breast or breasts if a mammogram screening demonstrates heterogeneously dense or extremely dense breast tissue when the woman’s primary healthcare provider or radiologist determines a comprehensive ultrasound screening is medically necessary.” “A breast ultrasound may be subject to any applicable copayment as required under a health benefit plan but shall not be subject to a deductible.”
“Insurance coverage for screening mammograms, including digital breast tomosynthesis (3D), and breast ultrasounds shall not prejudice coverage for diagnostic mammograms or breast ultrasounds as recommended by the woman’s physician.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To Top
California
Effective date: 4/1/2013; remains in effect through 1/1/2025 unless extended by law.
Who receives: Patient whose mammogram indicates heterogeneously or extremely dense breasts
How informed: In the letter sent to patients after their mammogram.
Notification required: “Your mammogram shows that your breast tissue is dense. Dense breast tissue is common and is not abnormal. However, dense breast tissue can make it harder to evaluate the results of your mammogram and may also be associated with an increased risk of breast cancer.
This information about the results of your mammogram is given to you to raise your awareness and to inform your conversations with your doctor. Together, you can decide which screening options are right for you. A report of your results was sent to your physician.”
Colorado
Effective date: 10/1/2017
Who receives: Patient whose mammogram indicates heterogeneously or extremely dense breasts.
How informed: In the letter sent to patients after their mammograms.
Notification required: “Your mammogram shows that your breast tissue is dense. Dense breast tissue is common and is not abnormal. However, dense breast tissue can make it harder to evaluate the results of your mammogram and may also be associated with an increased risk of breast cancer. This information about the results of your mammogram is given to you to raise your awareness and to inform your conversations with your doctor. Together, you can decide which screening options are right for you. A report of your results was sent to your physician.”
Insurance, effective 8/2/2019: applies to policies and contracts issued or renewed on or after 1/1/2021. “The coverage required must include a preventive breast cancer screening study that is within appropriate use guidelines as determined by the American College of Radiology, the National Comprehensive Cancer Network, or their successor entities, for the actual cost of an annual breast cancer screening using the noninvasive imaging modality appropriate for the covered person’s breast health needs, as determined by the covered person’s provider. For any breast imaging performed after the breast cancer screening study, whether it is diagnostic breast imaging for further evaluation or supplemental breast imaging within the same calendar year based on factors including a high lifetime risk for breast cancer or high breast density, the noninvasive imaging modality or modalities used must be the same as, or comparable to, the modality or modalities used for the breast cancer screening study.” “If the noninvasive imaging modality is recommended by the covered person’s provider and the breast imaging is within appropriate use guidelines as determined by the American College of Radiology, the National Comprehensive Cancer Network, or their successor entities, the covered person is not responsible for any cost-sharing amounts.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To Top
Connecticut
Effective date: 10/1/2009
Who receives: All women receive “information about breast density.” No further specifications are provided. The law additionally states that “where applicable” the notification below is required. “Where applicable” has been interpreted to mean women with heterogeneously or extremely dense breasts.
How informed: In the letter sent to patients after their mammogram.
Notification amendment, effective 10/1/2019: “If your mammogram demonstrates that you have dense breast tissue, which could hide small abnormalities, you might benefit from supplementary screening tests, which can include a breast ultrasound screening or a breast MRI examination, or both, depending on your individual risk factors. A report of your mammography results, which contains information about your breast density, has been sent to your physician’s or advanced practice registered nurse’s office and you should contact your physician or advanced practice registered nurse if you have any questions or concerns about this report.”
Notification required: “If your mammogram demonstrates that you have dense breast tissue, which could hide small abnormalities, you might benefit from supplementary screening tests, which can include a breast ultrasound screening or a breast MRI examination, or both, depending on your individual risk factors. A report of your mammography results, which contains information about your breast density, has been sent to your physician’s office and you should contact your physician if you have any questions or concerns about this report.”
Insurance amendment, effective 1/1/2023: Each individual health insurance policy providing coverage shall provide benefits for diagnostic and screening mammograms for insureds that are at least equal to the following minimum requirements: (A) A baseline mammogram, which may be provided by breast tomosynthesis at the option of the insured covered under the policy, for an insured who is: (i) Thirty-five to thirty-nine years of age, inclusive; or (ii) Younger than thirty-five years of age if the insured is believed to be at increased risk for breast cancer due to: (I) A family history of breast cancer; (II) Positive genetic testing for the harmful variant of breast cancer gene one, breast cancer gene two or any other gene variant that materially increases the insured’s risk for breast cancer; (III) Prior treatment for a childhood cancer if the course of treatment for the childhood cancer included radiation therapy directed at the chest; or (IV) Other indications as determined by the insured’s physician, advanced practice registered nurse, physician assistant, certified nurse midwife or other medical provider; and (B) Mammograms, which may be provided by breast tomosynthesis at the option of the insured covered under the policy, every year for an insured who is: (i) Forty years of age or older; or (ii) Younger than forty years of age if the insured is believed to be at increased risk for breast cancer due to: (I) A family history, or prior personal history, of breast cancer; (II) Positive genetic testing for the harmful variant of breast cancer gene one, breast cancer gene two or any other gene that materially increases the insured’s risk for breast cancer; (III) Prior treatment for a childhood cancer if the course of treatment for the childhood cancer included radiation therapy directed at the chest; or (IV) Other indications as determined by the insured’s physician, advanced practice registered nurse, physician assistant, certified nurse midwife or other medical provider.
Comprehensive diagnostic and screening ultrasounds of an entire breast or breasts if: (i) A mammogram demonstrates heterogeneous or dense breast tissue based on the Breast Imaging Reporting and Data System established by the American College of Radiology; or (ii) An insured is believed to be at increased risk for breast cancer due to: (I) A family history or prior personal history of breast cancer; (II) Positive genetic testing for the harmful variant of breast cancer gene one, breast cancer gene two or any other gene that materially increases the insured’s risk for breast cancer; (III) Prior treatment for a childhood cancer if the course of treatment for the childhood cancer included radiation therapy directed at the chest; or (IV) Other indications as determined by the insured’s physician, advanced practice registered nurse, physician’s assistant, certified nurse midwife or other medical provider.
Diagnostic and screening magnetic resonance imaging of an entire breast or breasts: (i) In accordance with guidelines established by the American Cancer Society for an insured who is thirty-five years of age or older; or (ii) If an insured is younger than thirty-five years of age and believed to be at increased risk for breast cancer due to: (I) A family history, or prior personal history, of breast cancer; (II) Positive genetic testing for the harmful variant of breast cancer gene one, breast cancer gene two or any other gene that materially increases the insured’s risk for breast cancer; (III) Prior treatment for a childhood cancer if the course of treatment for the childhood cancer included radiation therapy directed at the chest; or (IV) Other indications as determined by the insured’s physician, advanced practice registered nurse, physician’s assistant, certified nurse midwife or other medical provider.
Insurance amendment, effective 10/1/2021: Each individual health insurance policy providing coverage shall not impose a coinsurance, copayment, deductible or other out-of-pocket expense for such benefits.
Insurance amendment, effective 1/1/2020: “Both individual and group health insurance policies shall provide benefits for comprehensive ultrasound screening of an entire breast or breasts if: (i) a mammogram demonstrates heterogeneous or dense breast tissue based on the Breast Imaging Reporting and Data System established by the American College of Radiology; or if (ii) a woman is believed to be at increased risk for breast cancer due to (i) family history or prior personal history of breast cancer, (ii) positive genetic testing, or (iii) other indications as determined by a woman’s physician or advanced practice registered nurse; or (iii) such screening is recommended by a woman’s treating physician for a woman who (i) is forty years of age or older, (ii) has a family history or prior personal history of breast cancer, or (iii) has a prior personal history of breast disease diagnosed through biopsy as benign; and (b) magnetic resonance imaging of an entire breast or breasts in accordance with guidelines established by the American Cancer Society.”
No policy shall impose a coinsurance, copayment, deductible or other expenses that is more than $20 for such ultrasound screening.
Insurance, effective 10/1/2006: Both individual and group health insurance policies shall provide benefits for comprehensive ultrasound screening of an entire breast or breasts if a mammogram demonstrates (1) heterogeneous or dense breast tissue or (2) if a woman is believed to be at increased risk for breast cancer due to family history or prior personal history of breast cancer, positive genetic testing or other indications as determined by a woman’s physician or advanced practice registered nurse. Benefits must also include magnetic resonance imaging of an entire breast or breasts in accordance with guidelines established by the American Cancer Society.
No policy shall impose a copayment that is more than $20 for such ultrasound screening. Deductible is subject to the patient’s health care plan.
Expanded Mammography Coverage, effective 1/1/2017 (plus see amendments): State law requires insurance companies to provide coverage for screening 3D mammograms. Beginning 1/1/2019, state law requires insurance companies to provide coverage for diagnostic 2D or 3D mammograms. Beginning 1/1/2020, state law requires insurance coverage for a baseline mammogram (2D or 3D) for a woman 35 to 39 years of age. Beginning 1/1/2023, state law requires baseline mammograms for women younger than 35 if believed to be at increased risk. Annual mammograms 40+, or younger than 40 if believed to be at increased risk.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To Top
Delaware
Effective date: 12/21/2015
Who receives: All patients. Every patient will be provided information about their own breast density.
How Informed: In the letter sent to patients after their mammogram.
Notification required: None specifically required, however Delaware mammography facilities have been provided sample wording to use based on guidelines from the American College of Radiology (ACR). The notification will include the patient’s breast density based on the ACR Breast Imaging Reporting and Data System (BI-RADS), and awareness statements about breast density. It will also include notice to patients to use this information to guide discussions about screening with their referring physicians.
Insurance, effective 12/31/2024: All group and blanket health insurance policies which are delivered or issued for delivery by any health insurer or health service corporation and which provide benefits for outpatient services shall provide coverage for diagnostic breast examinations and supplemental breast screening examinations. The terms of such coverage, including cost-sharing requirements, shall be no less favorable than the cost-sharing requirements applicable to screening mammography for breast cancer. Exceptions apply.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To TopFlorida
Effective date: 7/1/2018; remains in effect through 9/10/2024 unless extended by law.
Who receives: Patient whose mammogram indicates heterogeneously or extremely dense breasts.
How informed: In the letter sent to patients after their mammogram.
Notification required: “Your mammogram shows that your breast tissue is dense. Dense breast tissue is relatively common and is found in approximately 50 percent of women. The presence of dense breast tissue can make it more difficult to detect some abnormalities in the breast and may also be associated with an increased risk of breast cancer. This information about the results of your mammogram is given to you to raise your awareness. A report of your results was sent to your health care provider. Further recommendations may be added at the discretion of the interpreting radiologist. Please be aware that additional screening studies may not be covered by your insurance.”
Back To TopGeorgia
Effective date: 7/1/2019
Who receives: Patient whose mammogram indicates heterogeneously or extremely dense breasts.
How informed: In the letter sent to patients after their mammogram.
Notification required: “Your mammogram shows that your breast tissue is dense. Dense breast tissue is very common and is not abnormal. However, dense breast tissue can make it more difficult to detect cancer through a mammogram. Also, dense breast tissue may increase your risk for breast cancer. This information about the result of your mammogram is given to you to increase your awareness. Use this information to talk with your health care provider about whether other supplemental tests in addition to your mammogram may be appropriate for you, based on your individual risk. A report of your results was sent to your ordering physician. If you are self-referred, a report of your results was sent to you in addition to this summary.”
Insurance amendment, effective 1/1/2024: Amends 1/1/2023 law (below) to “….implement the provisions…in accordance with current guidelines established by professional medical organizations such as the National Comprehensive Cancer Network.”
Insurance, effective 1/1/2023: “A health benefit policy that provides coverage for diagnostic examinations for breast cancer shall include provisions that ensure that the cost-sharing requirements applicable to diagnostic and supplemental breast screening examinations are no less favorable than the cost-sharing requirements applicable to screening mammography for breast cancer.” “’Supplemental breast screening examination’ means a medically necessary and clinically appropriate, as defined by the guidelines established by the National Comprehensive Cancer Network as of January 1, 2022, examination of the breast…”
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To Top
Hawaii
Effective date: 1/1/2014
Who receives: Patient whose mammogram indicates heterogeneously or extremely dense breasts
How informed: In the letter sent to patients after their mammogram.
Notification required: “Your mammogram shows that your breast tissue is dense. Dense breast tissue is very common and is not abnormal. However, dense breast tissue can make it harder to find cancer on a mammogram and may also be associated with an increased risk of breast cancer. This information about the result of your mammogram is given to you to raise your awareness. Use this information to talk to your physician as to whether, based on your risk, more screening tests might be useful. A report of your results was sent to your physician.”
Back To TopIdaho
No density notification or insurance legislation has been introduced.
Back To TopIllinois
Effective date: 1/1/2019
Who receives: Patient whose mammogram indicates heterogeneously or extremely dense breasts.
How informed: In the letter sent to patients after their mammogram.
Notification: A notice regarding breast density to patients with dense breast tissue substantially similar to the following: “Your mammogram indicates you have dense breast tissue. Dense breast tissue is normal and identified on mammograms in about 50% of women. Dense breast tissue can make it more difficult to detect cancer on a mammogram and may be associated with an increased risk for breast cancer. Despite these limitations, screening mammograms have been proven to save lives. Continue to have routine screening mammography whether or not additional exams are suggested for you. This information is provided to raise your awareness of the impact of breast density on cancer detection. For further information about dense breast tissue, as well as other breast cancer risk factors, contact your breast imaging health care provider.”
Education: A law was passed which directs, from funds made available for this purpose, publication of a summary outlining methods for the early detection and diagnosis of breast cancer. The brochure is to include the meaning and consequences of “dense breast tissue” under the guidelines of the Breast Imaging Reporting and Data System of the American College of Radiology. The Illinois Department of Health is to make the brochure available to the public. Effective date 1/1/2014.
Insurance, effective 1/1/2018: If a routine mammogram reveals heterogeneous or dense breast tissue, coverage must provide for a comprehensive ultrasound screening of an entire breast or breasts and MRI when determined to be medically necessary by a physician. Coverage shall be provided at no cost to the insured (i.e., co-pays or deductibles may not be applied) and shall not be applied to an annual or lifetime maximum benefit. When health care services are available through contracted providers and a person does not comply with plan provisions specific to the use of contracted providers, the coverage requirements are not applicable. When a person does not comply with plan provisions specific to the use of contracted providers, plan provisions specific to the use of non-contracted providers must be applied without distinction for coverage required and shall be at least as favorable as for other radiological examinations covered by the policy or contract.
Expanded Mammography Coverage, effective 7/1/2016: State law requires insurance companies to provide coverage for 3D mammograms; however, not all insurance policies are required to comply. Effective 1/1/2020, coverage for a diagnostic mammogram when medically necessary with no cost sharing (deductible, coinsurance, copayment, or other) to the patient.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To Top
Indiana
Notification amendment effective: 7/1/24
Who receives: All women receive notification telling them whether their breasts are “dense” or “not dense.”
How informed: In the letter sent to patients after their mammograms.
Notification required (if dense): “Breast tissue can either be dense or not dense. Dense tissue makes it harder to find breast cancer on a mammogram and also raises the risk of developing breast cancer. Your breast tissue is not dense. Talk to your health care provider about breast density, risks for breast cancer, and your individual situation.”.
Original notification effective date: 7/1/16
Who receives: Unclear. Law specifies that if imaging facility determines patient has “an amount of breast and connective tissue in comparison to fat in the breast,” the facility shall notify the patient of the determination. However, imaging facilities are not required to make a determination of the amount of breast and connective tissue in comparison to fat in the breast. Further, all breasts have an amount of breast/connective tissue in comparison to fat.
Notification required: Not specified. The law only requires a patient be told they have “an amount of breast and connective tissue in comparison to fat in the breast.” The law does not provide specific guidelines, suggest/recommend reporting language or require that a patient be provided information about personal breast density or breast density in general.
PLEASE NOTE: State legislative language can be vague or complex and is open to interpretation. For interpretation from the Medical Licensing Board of Indiana click here.
Insurance: A state employee health plan, an individual contract or group contract for insurance that provides coverage for basic health care services, and a policy of accident and sickness insurance must each provide coverage for appropriate medical screening, test, or examination for a female insurance enrollee who is at least forty (40) years of age and who has been determined to have high breast density. High breast density means a condition in which there is a greater amount of breast and connective tissue in comparison to fat in the breast. Additional screening subject to the copay and deductible of patient’s health care plan.
There are exceptions to this coverage. No coverage is required for the following types of insurance:
(1) Accident only, credit, dental, vision, Medicare supplement, long-term care, or disability income insurance.
(2) Coverage issued as a supplement to liability insurance.
(3) Automobile medical payment insurance.
(4) A specified disease policy.
(5) A short term insurance plan that:
a. may not be renewed; and
b. has a duration of not more than six (6) months.
(6) A policy that provides indemnity benefits not based on any expense incurred requirement, including a plan that provides coverage for:
a. hospital confinement, critical illness, or intensive care; or
b. gaps for deductibles or copayments.
(7) Worker’s compensation or similar insurance.
(8) A student health plan.
(9) A supplemental plan that always pays in addition to other coverage.
(10) An employer sponsored health benefit plan that is:
a. provided to individuals who are eligible for Medicare; and
b. not marketed as, or held out to be, a Medicare supplement policy
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To Top
Iowa
Effective date: 11/15/2017
Who receives: Every patient must receive information that identifies the patient’s individual breast density classification (fatty, scattered, heterogeneously dense or extremely dense). Patients with heterogeneously or extremely dense breasts receive additional notification below.
How informed: In the letter sent to patients after their mammogram.
Notification required: The notification to the patient shall include evidence-based information on dense breast tissue, the increased risk associated with dense breast tissue, and the effects of dense breast tissue on screening mammography and shall be stated in a language appropriate for the facility’s patient population.
Back To TopKansas
A bill was introduced in 2012 but did not progress and/or pass into law.
Back To TopKentucky
Effective date: 7/1/2017 in effect through 1/1/2021. Reinstated 7/1/2021 (estimated) in effect through 1/1/2025.
Who receives: Patient whose mammogram indicates heterogeneously or extremely dense breasts.
How informed: In the letter sent to patients after their mammogram.
Notification required: “Your x-ray mammogram shows that your breast tissue is dense. Dense breast tissue is common among women and is not abnormal. However, women with dense breast tissue may have a slightly increased risk for developing breast cancer. Dense breast tissue may also make it more difficult to detect an early breast cancer on your x-ray mammogram. At this time, there are no specific recommendations for additional screening or other measures related to having dense breast tissue. However, you may want to talk to your doctor about other ways that you might be able to reduce your risk of breast cancer. A report of your results was sent to your ordering physician. If you are self-referred, a report of your results was sent to you in addition to this summary.”
Insurance, effective 1/1/2025: “A health insurance policy, plan, certificate, or contract issued, renewed or delivered….Shall not impose any cost-sharing requirements for any diagnostic breast examination or supplement breast examination [to include, but not limited to MRI or ultrasound], that is covered under the policy, plan, certificate or contract.” Exceptions apply.
Expanded Mammography Coverage: State law expands definition of “mammogram” to include digital mammography including breast tomosynthesis (3D mammograms).
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To Top
Louisiana
Effective date: 1/1/2016
Who receives: All patients. This law does not require women be provided information as to whether they have dense breasts. Patients with and without dense breasts receive the same notification.
How informed: In the letter sent to patients after their mammogram.
Notification required: “If your mammogram demonstrates that you have dense breast tissue, which could hide abnormalities, and you have other risk factors for breast cancer that have been identified, you might benefit from supplemental screening tests that may be suggested by your ordering physician. Dense breast tissue, in and of itself, is a relatively common condition. Therefore, this information is not provided to cause undue concern, but rather to raise your awareness and to promote discussion with your physician regarding the presence of other risk factors, in addition to dense breast tissue. A summary of your mammography results will be sent to you, and a full mammography report will be sent to your physician and also to you. You should contact your physician if you have any questions or concerns regarding your summary or report of results.”
Insurance amendment, effective 1/1/2022: “Minimum mammography examination” means mammographic examinations, including but not limited to digital breast tomosynthesis (DBT), performed no less frequently than the following schedule and criteria of the American Society of Breast Surgeons provides:
(a)(i) Except as provided in this Subparagraph, one baseline mammogram for any woman who is thirty-five through thirty-nine years of age.
(ii) For women with a hereditary susceptibility from pathogenic mutation carrier status or prior chest wall radiation, an annual MRI starting at age twenty-five and annual mammography (DBT preferred modality) starting at age thirty. Such examinations shall be in accordance with recommendations by National Comprehensive Cancer Network guidelines or the American Society of Breast Surgeons Position Statement on Screening Mammography no later than the following policy or plan year following changes in the recommendations.
(iii) Annual mammography (DBT preferred modality) and access to supplemental imaging (MRI preferred modality) starting at age thirty-five upon recommendation by her physician if the woman has a predicted lifetime risk greater than twenty percent by any validated model published in peer reviewed medical literature.
(b) Annual mammography (DBT preferred modality) for any woman who is forty years of age, or older.
(i) Consideration given to supplemental imaging (breast ultrasound initial preferred modality, followed by MRI if inconclusive), if recommended by her physician, for women with increased breast density (C and D density).
(ii) Access to annual supplemental imaging (MRI preferred modality), if recommended by her physician, for women with a prior history of breast cancer below the age of fifty or with a prior history of breast cancer at any age and dense breast (C and D density).
(iii) Any coverage provided pursuant to this Subsection may be subject to the health coverage plan’s utilization review using guidelines published in peer reviewed medical literature consistent with this Section.
Insurance, effective 1/1/2021: “Any health coverage plan delivered or issued for delivery shall include coverage for diagnostic imaging at the same level of coverage provided for the minimum mammography examination pursuant to R.S. 22:1028.” “The health coverage plan may require a referral by the treating physician based on medical necessity for the diagnostic imaging to be eligible for the coverage required.” “Any coverage required pursuant to the provisions of this Section shall not be subject to any policy or health coverage plan deductible amount.” ‘”Diagnostic imaging’ means a diagnostic mammogram or breast ultrasound screening for breast cancer designed to evaluate an abnormality in the breast that is any of the following: (a) Seen or suspected from a screening examination for breast cancer. (b) Detected by another means of examination. (c) Suspected based on the medical history or family medical history of the individual.”
Expanded Mammography Coverage, effective 1/1/2019
State law expands definition of “mammography” to include digital mammography or breast tomosynthesis (3D mammograms).
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To TopMaine
Bill Number: LD 550
This bill was introduced in the 2017 legislative session, but did not progress and/or pass into law. However, in 2012, a state Work Group was formed to discuss the issue. The Group recommended Maine radiologists voluntarily communicate information about breast density to women with heterogeneously or extremely dense breasts in the letter sent to them after their mammograms.
The Work Group suggested radiologists may use or adapt the following language:
“The mammogram shows that your breast tissue is dense. Dense breast tissue is very common and is not abnormal. But dense breast tissue can make it harder to find cancer on a mammogram. Also, dense breast tissue may increase your breast cancer risk. This information about the result of your mammogram report is given to you to raise your awareness. Use this report when you talk to your doctor about your own risks for breast cancer, which includes your family history. At that time, ask your doctor if more screening tests might be useful, based on your risk.”
Insurance, effective 1/1/2024: All individual and group coverage subject to this law may not impose any cost-sharing requirements on a screening mammogram, diagnostic breast examination or supplemental breast examination (mammography, MRI, US) performed by a provider. Exceptions apply.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To TopMaryland
Effective date: 10/1/2013, amendment effective 10/1/2017
Who receives: All patients. This law does not require women be provided information as to whether they have dense breasts. Patients with and without dense breasts receive the same notification.
How informed: In the letter sent to patients after their mammogram.
Notification required effective 10/1/2017: “This notice contains the results of your recent mammogram, including information about breast density. If your mammogram shows that your breast tissue is dense, you should know that dense breast tissue is a common finding and is not abnormal, with about half of women having dense or highly dense breasts. However, dense breast tissue can make it harder to find cancer on a mammogram and may also be associated with an increased risk of cancer.
This information about the results of your mammogram is given to you to raise your awareness and to inform your conversations with your physician. Together, you can decide whether additional screening options are right for you based on your mammogram results, individual risk factors, or physical examination. A report of your results was sent to your physician.”
Insurance, effective 1/1/2024: The law prohibits, “… except under certain circumstances, insurers, nonprofit health service plans, and health maintenance organizations that provide coverage for diagnostic and supplemental breast examinations from imposing a copayment, coinsurance, or deductible requirement for the examination.” ‘Supplemental breast examination” means a medically necessary examination of the breast that is used to screen for breast cancer when: 1. There is no abnormality seen or suspected, 2. There is a personal or family medical history or additional factors that may increase an individual’s risk of breast cancer.” “Supplemental breast examination” includes an examination using breast magnetic resonance imaging or breast ultrasound.
Expanded Mammography Coverage, effective 1/1/2018: State law requires insurance companies to provide coverage for digital tomosynthesis (3D mammograms).
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To Top
Massachusetts
Effective date: 1/1/2015
Who receives: Patient whose mammogram indicates dense tissue.
How informed: In the letter sent to patients after their mammogram.
Notification required: There is no mandatory language that must be included. However, the notification has to include, at the minimum:
(1) that the patient’s mammogram shows dense breast tissue;
(2) that the degree of density apparent and an explanation of that degree of density;
(3) that dense breast tissue is common and not abnormal but that dense breast tissue may increase the risk of breast cancer;
(4) that dense breast tissue can make it more difficult to find cancer on a mammogram and that additional testing may be needed for reliable breast cancer screening;
(5) that additional screening may be advisable and that the patient should discuss the results of the mammogram with the patient’s referring physician or primary care physician;
(6) that the patient has the right to discuss the results of the patient’s mammogram with the interpreting radiologist or the referring physician;
(7) that a report of the patient’s mammogram has been sent to the referring physician and will become part of the patient’s medical record; and
(8) where the patient can find additional information about dense breast tissue.
Michigan
Effective date: 6/1/2015
Who receives: Patient whose mammogram indicates heterogeneously or extremely dense breasts.
How informed: In the letter sent to patients after their mammogram.
Notification required: “Your mammogram shows that your breast tissue is dense. Dense breast tissue is very common and is not abnormal. However, dense breast tissue can make it harder to find cancer through a mammogram. Also, dense breast tissue may increase your risk for breast cancer. This information about the result of your mammogram is given to you to raise your awareness. Use this information to discuss with your health care provider whether other supplemental tests in addition to your mammogram may be appropriate for you, based on your individual risk. A report of your results was sent to your ordering physician. If you are self-referred, a report of your results was sent to you in addition to this summary.”
Back To TopMinnesota
Effective date: 7/1/2014
Who receives: Patient whose mammogram indicates heterogeneously or extremely dense breasts.
How informed: In the letter sent to patients after their mammogram. The letter must include notice that the patient has dense tissue, that this may make it more difficult to detect cancer on a mammogram, and that this may increase her risk of breast cancer.
Notification which may be used: “Your mammogram shows that your breast tissue is dense. Dense breast tissue is relatively common and is found in more than 40 percent of women. However, dense breast tissue may make it more difficult to identify precancerous lesions or cancer through a mammogram and may also be associated with an increased risk of breast cancer. This information about the results of your mammogram is given to you to raise your own awareness and to help inform your conversations with your treating clinician who has received a report of your mammogram results. Together you can decide which screening options are right for you based on your mammogram results, individual risk factors, or physical examination.”
Insurance, effective 1/1/2024: If a health care provider determines an enrollee requires additional diagnostic services or testing after a mammogram, a health plan must provide coverage for the additional diagnostic services or testing with no cost-sharing, including co-pay, deductible, or coinsurance. Exceptions apply.
Expanded Mammography Coverage, effective 1/1/2020: Coverage for a preventative screening mammogram includes digital breast tomosynthesis for enrollees at risk for breast cancer and is covered as a preventative item. “At risk for breast cancers” means: (1) having a family history with one or more first- or second-degree relatives with breast cancer; (2) testing positive for BRCA 1 or BRCA 2 mutations; (3) having heterogeneously dense breasts or extremely dense breasts based on the Breast Imaging Reporting and Data System established by the American College of Radiology; or (4) having a previous diagnosis of breast cancer. Nothing prohibits a policy, plan, certificate, or contract from covering digital breast tomosynthesis for an enrollee who is not at risk for breast cancer.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To Top
Mississippi
Bill Number: SB2006
This bill was introduced in the 2017 legislative session and signed into law, however the amended/final language did not include any specific mention of/about breast density or requirement for density notification.
Back To TopMissouri
Effective date: 1/1/2015
Who receives: All patients, regardless of breast density. This law does not require women be provided information as to whether they have dense breasts.
How informed: While the law requires notification to be provided to the patient after her mammogram, it does not state how. Most other state laws, for instance, specifically require breast density information to be included in the letter sent to patients after their mammogram.
Notification required: “If your mammogram demonstrates that you have dense breast tissue, which could hide abnormalities, and you have other risk factors for breast cancer that have been identified, you might benefit from supplemental screening tests that may be suggested by your ordering physician. Dense breast tissue, in and of itself, is a relatively common condition. Therefore, this information is not provided to cause undue concern, but rather to raise your awareness and to promote discussion with your physician regarding the presence of other risk factors, in addition to dense breast tissue. A report of your mammography results will be sent to you and your physician. You should contact your physician if you have any questions or concerns regarding this report.”
Insurance, effective 1/1/2024: “This act prohibits cost-sharing requirements under coverage provided for diagnostic breast examinations, supplemental breast examinations, or low-dose mammography screenings.” Exceptions apply.
Insurance, effective 8/28/2020 but subject to individual policy applicability dates. Includes coverage for:
1. A mammogram every year for any woman deemed by a treating physician to have an above-average risk for breast cancer in accordance with the American College of Radiology guidelines for breast cancer screening;
2. Any additional or supplemental imaging, such as breast magnetic resonance imaging or ultrasound, deemed medically necessary by a treating physician for proper breast cancer screening or evaluation in accordance with applicable American College of Radiology guidelines; and
3. Ultrasound or magnetic resonance imaging services, if determined by a treating physician to be medically necessary for the screening or evaluation of breast cancer for any woman deemed by the treating physician to have an above-average risk for breast cancer in accordance with American College of Radiology guidelines for breast cancer screening.
Copay/deductible/co-insurance may apply.
Expanded Mammography Coverage, effective 1/1/2019: State law expands definition of “mammography” to include digital mammography or breast tomosynthesis (3D mammograms).
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To Top
Montana
Montana does not have a density “inform” law.
Insurance, effective 10/1/2023: “…a group health plan or a health insurance issuer offering group or individual health insurance coverage may not impose any cost-sharing requirements for a diagnostic breast examination or supplemental breast examination when the plan or coverage provides screening benefits, supplemental breast examinations, and diagnostic breast examinations furnished to an individual enrolled under the plan or coverage.” “Supplemental breast examination” means a medically necessary and clinically appropriate examination of the breast using breast magnetic resonance imaging or breast ultrasound that is: (a) used to screen for breast cancer when there is no abnormality seen or suspected; and (b) based on personal or family medical history or additional factors that may increase the individual’s risk of breast cancer.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To TopNebraska
Effective date: 7/24/2017
Who receives: Every patient must receive information that identifies the patient’s individual breast density classification (fatty, scattered, heterogeneously dense or extremely dense). Patients with heterogeneously or extremely dense breasts shall receive a notice substantially similar to the notification below.
How informed: In the letter sent to patients after their mammogram.
Notification required: The summary of the mammography report shall include a notice substantially similar to the following: “Your mammogram indicates that you have dense breast tissue. Dense breast tissue is a normal finding that is present in about forty percent of women. Dense breast tissue can make it more difficult to detect cancer on a mammogram and may be associated with a slightly increased risk for breast cancer. This information is provided to raise your awareness of the impact of breast density on cancer detection and to encourage you to discuss this issue, as well as other breast cancer risk factors, with your health care provider as you decide together which screening options may be right for you.”
Insurance, effective 1/1/2024: Any individual or group sickness and accident insurance policy or subscriber contract delivered, issued for delivery, or renewed in this state and any hospital, medical, or surgical expense-incurred policy, except for policies that provide coverage for a specified disease or other limited- benefit coverage, and (b) any self-funded employee benefit plan to the extent not preempted by federal law shall include coverage for screening mammography, digital breast tomosynthesis, bilateral whole breast ultrasound, and diagnostic magnetic resonance imaging as follows: (i) For a woman who is thirty-five years of age or older but younger than forty years of age, one base-line mammogram between thirty-five and forty years of age; (ii) For a woman who is younger than forty years of age and who, based on the National Comprehensive Cancer Network Guidelines for Breast Cancer Screening and Diagnosis version 1.2022 and the recommendation of the woman’s health care provider, has an increased risk of breast cancer due to (A) a family or personal history of breast cancer or prior atypical breast biopsy, (B) positive genetic testing, or (C) heterogeneous or dense breast tissue based on a breast imaging, at least one mammogram each year and additional mammograms if necessary; (iii) For a woman who is forty years of age or older, one mammogram every year; (iv) For a woman who, based on the National Comprehensive Cancer Network Guidelines for Breast Cancer Screening and Diagnosis version 1.2022 and the recommendation of the woman’s health care provider, has an increased risk for breast cancer due to (A) a family or personal history of breast cancer or prior atypical breast biopsy, (B) positive genetic testing, or (C) heterogeneous or dense breast tissue based on a breast imaging, one digital breast tomosynthesis each year; (v) For a woman who, based on the National Comprehensive CancerNetwork Guidelines for Breast Cancer Screening and Diagnosis version 1.2022 and the recommendation of the woman’s health care provider, has an increased risk for breast cancer due to (A) a family or personal history of breast cancer or prior atypical breast biopsy, (B) positive genetictesting, or (C) heterogeneous or dense breast tissue based on a breast imaging, one bilateral whole breast ultrasound each year; (vi) For a woman who, based on the National Comprehensive Cancer Network Guidelines for Breast Cancer Screening and Diagnosis version 1.2022 and the recommendation of the woman’s health care provider, has an increased risk for breast cancer due to (A) a family or personal history of breast cancer or prior atypical breast biopsy, (B) positive genetic testing, or (C) a history of chest radiation, one diagnostic magnetic resonance imaging each year; and (vii) For a woman who, based on national standard risk models or the National Comprehensive Cancer Network Guidelines for Breast Cancer Screening and Diagnosis, has an increased risk of breast cancer and heterogeneous or dense breast tissue, one diagnostic magnetic resonance imaging each year.” Out-of-pocket costs prohibited except for MRI if only risk is breast density. Exceptions apply.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To Top
Nevada
Effective date: 1/1/2014, but notification language amended to the following effective 7/1/2015
Who receives: All patients. Every patient must receive a statement of the category of their own breast density. Patients with “dense” breasts must also receive the notification below.
How informed: In the letter sent to patients after their mammogram.
Notification required: “Your mammogram shows that your breast tissue is dense. Dense breast tissue is common and is not abnormal. However, dense breast tissue can make it harder to evaluate the results of your mammogram and may also be associated with an increased risk of breast cancer. This information about the results of your mammogram is given to you to raise your awareness and to inform your conversations with your physician. Together, you can decide which screening options are right for you. A report of your results was sent to your physician.”
Back To TopNew Hampshire
A bill was introduced but did not progress and/or pass into law by end of the 2016 legislative session.
Expanded Mammography Coverage, effective 8/7/18: State law expands definition of “mammography” to include digital mammography or breast tomosynthesis (3D mammograms).
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To Top
New Jersey
Effective date: 5/1/2014
Who receives: All patients, regardless of breast density. This law does not require women be provided information as to whether they have dense breasts.
How informed: In the letter sent to patients after their mammogram.
Notification required:
“Your mammogram may show that you have dense breast tissue as determined by the Breast Imaging Reporting and Data System established by the American College of Radiology. Dense breast tissue is very common and is not abnormal. However, in some cases, dense breast tissue can make it harder to find cancer on a mammogram and may also be associated with a risk factor for breast cancer. Discuss this and other risks for breast cancer that pertain to your personal medical history with your health care provider. A report of your results was sent to your health care provider. You may also find more information about breast density at the website of the American College of Radiology, www.acr.org.”
Insurance: No medical or health service corporation contract or health insurance policy and every individual and small employer health benefit and health maintenance organization providing hospital or medical expense benefits shall be delivered, issued, executed, or renewed unless the contract provides benefits to any subscriber or other person covered thereunder for expenses incurred in conducting an ultrasound evaluation, a magnetic resonance imaging scan, a three-dimensional mammography, or other additional testing of an entire breast or breasts, after a baseline mammogram examination, if the mammogram is abnormal within any degree of breast density including not dense, moderately dense, heterogeneously dense, or extremely dense breast tissue, or if the patient has additional risk factors for breast cancer including but not limited to family history of breast cancer, prior personal history of breast cancer, positive genetic testing, extremely dense breast tissue based on the Breast Imaging Reporting and Data System established by the American College of Radiology and Data System established by the American College of Radiology, or other indications as determined by the patient’s health care provider. Additional screening subject to the copay and deductible of patient’s health care plan.
Expanded Mammography Coverage, effective 8/1/2018: State law requires insurance companies to provide coverage for digital tomosynthesis (3D mammograms) in women 40 and over with no deductible, coinsurance or other cost sharing, and in the case of digital tomosynthesis conducted for diagnostic purposes in women of any age.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To Top
New Mexico
Effective date: 7/1/2019
Who receives: Every patient must receive information that identifies the patient’s individual breast density classification (fatty, scattered, heterogeneously dense or extremely dense). Patients with heterogeneously or extremely dense breasts must receive the notification below.
How informed: In the letter sent to patients after their mammogram.
Notification required: “Your mammogram indicates that you have dense breast tissue. Dense breast tissue is common and is not abnormal. However, dense breast tissue may make it harder to evaluate the results of your mammogram. It may also be associated with an increased risk of breast cancer. This information is being provided to raise your awareness and to inform your conversation with your health care provider. Together, you can decide if additional screening options may be right for you. A report of your results was sent to your health care provider.”
Insurance, effective 1/1/2024: “An individual or group health insurance policy, health care plan or certificate of insurance that is delivered, issued for delivery or renewed in this state that provides coverage for diagnostic and supplemental breast examinations shall not impose cost sharing for diagnostic and supplemental breast examinations.” “Supplemental breast examination” means a medically necessary and clinically appropriate examination of the breast using breast magnetic resonance imaging or breast ultrasound that is: (a) used to screen for breast cancer when there is no abnormality seen or suspected; and (b) based on personal or family medical history or additional factors that may increase the individual’s risk of breast cancer. Exceptions apply.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To TopNew York
Effective date: 1/19/2013
Who receives: Patient whose mammogram indicates heterogeneously or extremely dense breasts.
How informed: In the letter sent to patients after their mammogram.
Notification required: “Your mammogram shows that your breast tissue is dense. Dense breast tissue is very common and is not abnormal. However, dense breast tissue can make it harder to find cancer on a mammogram and may also be associated with an increased risk of breast cancer.
This information about the result of your mammogram is given to you to raise your awareness. Use this information to talk to your doctor about your own risks for breast cancer. At that time, ask your doctor if more screening tests might be useful, based on your risk. A report of your results was sent to your physician.”
Insurance, effective 1/1/2017. In part, it amends/adds the following to current insurance law: “Screening and diagnostic imaging for the detection of breast cancer, including diagnostic mammograms, breast ultrasounds, or magnetic resonance imaging, covered under the policy shall not be subject to annual deductibles or coinsurance.” “The requirement only applies with respect to participating providers in the insurer’s network, or with respect to non- participating providers, if the insurer does not have a participating provider in the in-network benefits portion of its network with the appropriate training and experience to meet the particular health care needs of the insured.”
A further action clarified “Tomosynthesis is a screening and diagnostic imaging tool for the detection of breast cancer that is covered by these provisions. Therefore, an issuer must cover tomosynthesis, when medically necessary, without being subject to annual deductibles or coinsurance.”
Expanded Mammography Coverage, effective 9/1/2019: For large group policies that provide coverage for hospital, surgical or medical care an annual mammogram for covered persons aged thirty-five through thirty-nine, inclusive, upon the recommendation of a physician, subject to the insurer’s determination that the mammogram is medically necessary. This coverage is not subject to annual deductibles or coinsurance.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To TopNorth Carolina
Effective date: 1/1/2014
Who receives: Every patient must receive information that identifies the patient’s individual breast density classification (fatty, scattered, heterogeneously dense or extremely dense). Patients with heterogeneously or extremely dense breasts must receive the notification below.
How informed: In the letter sent to patients after their mammogram.
Notification required: “Your mammogram indicates that you may have dense breast tissue. Dense breast tissue is relatively common and is found in more than forty percent (40%) of women. The presence of dense tissue may make it more difficult to detect abnormalities in the breast and may be associated with an increased risk of breast cancer. We are providing this information to raise your awareness of this important factor and to encourage you to talk with your physician about this and other breast cancer risk factors. Together, you can decide which screening options are right for you. A report of your results was sent to your physician.”
Back To TopNorth Dakota
Effective date: This law has expired. Signed into law 4/8/15 and in effect until 7/31/17.
Who receives: Patient whose mammogram indicates heterogeneously or extremely dense breasts.
How informed: In the letter sent to patients after their mammogram.
Notification: The summary of the written report that is sent to the patient shall include notice that the patient has dense breast tissue, that this dense breast tissue may make it more difficult to detect cancer on a mammogram, and that this dense breast tissue may increase the patient’s risk of breast cancer.
Back To TopOhio
Effective date: 3/19/2015
Who receives: Women whose mammogram indicates dense tissue
How informed: In the letter sent to patients after their mammogram.
Notification amendment, effective 9/23/2022: “Your mammogram shows that your breast tissue is dense. Dense breast tissue is very common and is not abnormal. However, dense breast tissue can make it harder to find cancer on a mammogram and also may increase your risk of developing breast cancer. Because you have dense breast tissue, you could benefit from additional imaging tests such as a screening breast ultrasound or breast magnetic resonance imaging. This information about your breast density is being provided to you to raise your awareness. It is important to continue routine screening mammograms and use this information to speak with your health care provider about your own risk for breast cancer. At that time, ask your health care provider if more screening tests might be useful based on your risk. A report of your mammogram results was sent to your health care provider.”
Notification required: “Your mammogram demonstrates that you have dense breast tissue, which could hide abnormalities. Dense breast tissue, in and of itself, is a relatively common condition. Therefore, this information is not provided to cause undue concern; rather, it is to raise your awareness and promote discussion with your health care provider regarding the presence of dense breast tissue in addition to other risk factors.
Insurance, effective 9/23/2022: “’Supplemental breast cancer screening’ means any additional screening method deemed medically necessary by a treating health care provider for proper breast cancer screening in accordance with applicable American college of radiology guidelines, including magnetic resonance imaging, ultrasound, or molecular breast imaging.” “The benefits…shall cover expenses for supplemental breast cancer screening for an adult woman who meets either of the following conditions: (a) The woman’s screening mammography demonstrates, based on the breast imaging reporting and data system established by the American College of Radiology, that the woman has dense breast tissue; (b) The woman is at an increased risk of breast cancer due to family history, prior personal history of breast cancer, ancestry, genetic predisposition, or other reasons as determined by the woman’s health care provider.” Deductibles and copayments still apply.
Expanded Mammography Coverage, effective 9/23/2022: Screening mammography includes digital breast tomosynthesis.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To Top
Oklahoma
Effective date: 11/1/2016
Who receives: Every patient must receive information that identifies the patient’s individual breast density classification. Patients with heterogeneously or extremely dense breasts must receive the notification below.
How informed: In the letter sent to patients after their mammogram.
Notification required: “Your mammogram indicates that you have dense breast tissue. Dense breast tissue is common and is found in more than fifty percent (50%) of women and is not abnormal. However, dense breast tissue may make it more difficult to detect breast cancer and may be associated with an increased risk of breast cancer. This information is being provided to raise your awareness and to encourage you and your health care provider to discuss this and other breast cancer risk factors. Together, you and your health care provider can decide if additional screening options may be right for you. A report of your results was sent to your health care provider.”
Insurance, effective 11/1/2022: “All health benefit plans shall include the coverage…for a low-dose mammography screening for the presence of occult breast cancer and a diagnostic examination for breast cancer. Such coverage shall not: 1. Be subject to the policy deductible, co-payments and co-insurance limits of the plan; or 2. Require that a female undergo a mammography screening at a specified time as a condition of payment… Any female thirty-five (35) through thirty-nine (39)years of age shall be entitled pursuant to the provisions of this section to coverage for a low-dose mammography screening once every five (5) years… Any female forty (40) years of age or older shall be entitled pursuant to the provisions of this section to coverage for an annual low-dose mammography screening.”
Expanded Mammography Coverage, effective 11/1/2018: State law expands definition of “mammography” to include digital mammography or breast tomosynthesis (3D mammograms).
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To Top
Oregon
Effective date: 1/1/2014
Who receives: Notification is required to only those patients who have extremely dense breasts. For patients with heterogeneously dense breasts, the decision of whether or not to send the patient notification is left to the interpreting radiologist.
How informed: In the letter sent to patients after their mammogram.
Notification required: “Your mammogram shows that your breast tissue is dense. For most women, breast density decreases with age, but in some women, there is little change. Dense breast tissue is common and is not abnormal. However, dense breast tissue can make it harder to find cancer on a mammogram and may also be associated with an increased risk of breast cancer. This information is provided to you by Oregon State Law to raise your awareness and to promote discussion with your health care provider about your own risk for breast cancer. Together, you can decide if additional breast imaging tests such as a breast ultrasound, Magnetic Resonance Imaging (MRI) or Breast-Specific-Gamma-Imaging (BSGI) would be beneficial based on your risk factors and physical examinations. A report of your results was sent to your health care provider.”
Insurance, effective date 1/1/2024: A carrier offering a group health benefit plan or an individual health benefit plan that reimburses the cost of supplemental (such as MRI, US) or diagnostic breast examinations using mammo, MRI, US, may not impose out-of-pocket expenses on the coverage of a medically necessary supplemental or diagnostic breast examination. Exceptions apply.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To TopPennsylvania
Effective date: 1/30/2014
Who receives: All patients will receive information about their individual breast density and all patients receive the required notification below.
How informed: In the letter sent to patients after their mammogram.
Notification required: “This notice contains the results of your recent mammogram, including information about breast density. If your mammogram shows that your breast tissue is dense, you should know that dense breast tissue is a common finding and is not abnormal. Statistics show many patients could have dense or highly dense breasts. Dense breast tissue can make it harder to find cancer on a mammogram and may be associated with an increased risk of cancer. This information about the result of your mammogram is given to you to raise your awareness and to inform your conversations with your physician. Together, you can decide which screening options are right for you, based on your mammogram results, individual risk factors or physical examination. A report of your results was sent to your physician.”
Insurance amendment, effective on plan renewals but no later than 1/1/2025: All costs associated with one supplemental breast screening every year (see qualifying reasons below) and genetic testing/counseling. For effective date by insurance type, see here.
Insurance, effective 8/30/2020 but subject to individual policy applicability dates: Supplemental MRI or, if such imaging is not possible, ultrasound if recommended by the treating physician if woman is believed to be at an increased risk of breast cancer due to:
(1) Personal history of atypical breast histologies;
(2) personal history or family history of breast cancer;
(3) genetic predisposition for breast cancer;
(4) prior therapeutic thoracic radiation therapy;
(5) heterogeneously dense breast tissue based on breast composition categories of the breast imaging and reporting data system established by the American College of Radiology with any one of the following risk factors: (i) lifetime risk of breast cancer of greater than 20%, according to risk assessment tools based on family history; (ii) personal history of BRCA1 or BRCA2 gene mutations; (iii) first-degree relative with a BRCA1 or BRCA2 gene mutation but not having had genetic testing herself; (iv) prior therapeutic thoracic radiation therapy between 10 and 30 years of age; or (v) personal history of Li-Fraumeni syndrome, Cowden Syndrome or Bannayan-Riley-Ruvalcaba Syndrome or a first-degree relative with one of these syndromes.
(6) extremely dense breast tissue based on breast composition categories of the Breast Imaging and Reporting Data System established by the American College of Radiology.
Copay/deductible/co-insurance may apply.
Expanded Mammography Coverage, effective 10/1/2015: State law expands definition of “mammography” to include digital mammography or breast tomosynthesis (3D mammograms).
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To TopRhode Island
Effective date: 10/1/2014
Who receives: All patients. Every patient will be provided information that identifies the patient’s individual breast tissue classification (fatty, scattered, heterogeneously dense or extremely dense).
How informed: In the letter sent to patients after their mammogram. Patients with heterogeneously or extremely dense breasts must receive the notification below.
Notification required: “Your mammogram indicates that you have dense breast tissue. Dense breast tissue is relatively common and is found in about forty percent (40%) of women. The presence of dense tissue can make it more difficult to detect cancers in the breast by mammography because it can hide small abnormalities and may be associated with an increased risk. Hence, you may benefit from supplementary screening tests, which may include a breast ultrasound screening, or a breast MRI examination, or both, depending on your individual risk factors.
We are providing this information to raise your awareness of this important factor and to encourage you to discuss your dense breast tissue, as well as other breast cancer risk factors, with your health care provider. Together, you can decide which screening options are right for you.
A report of your results was sent to your physician. You should contact your physician if you have any questions or concerns about this report.”
Insurance, effective, 01/01/2024: Coverage for two screening mammograms per year when recommended by a physician for women who have been treated for breast cancer within the last five (5) years or who are at high risk of developing breast cancer due to genetic predisposition (BRCA gene mutation or multiple first degree relatives) or high-risk lesion on prior biopsy (lobular carcinoma in situ or atypical ductal hyperplasia). Coverage also for any screening deemed medically necessary for proper breast cancer screening in accordance with applicable American College of Radiology guidelines including, but not limited to, magnetic resonance imaging, ultrasound, or molecular breast imaging for any person who has received notice of the existence of dense breast tissue. Copays/deductibles apply.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To TopSouth Carolina
Effective date: 5/12/2016
Who receives: Law does not state specifically, but notes that “where applicable,” the report must include the notification.
How informed: In the letter sent to patients after their mammograms.
Notification required: “Your mammogram shows that your breast tissue is dense. Dense tissue is common and is not abnormal. However, dense breast tissue can make it harder to evaluate the results of your mammogram and may also be associated with an increased risk of breast cancer. This information about the results of your mammogram is given to you to raise your awareness and to inform your conversations with your doctor. Together, you can decide which screening options are right for you. A report of your results was sent to your physician.”
Back To TopSouth Dakota
Effective date: 7/1/2019
Who receives: Every patient must receive information that identifies the patient’s individual breast density classification (fatty, scattered, heterogeneously dense or extremely dense). Patients with heterogeneously or extremely dense breasts must receive the notification below.
How informed: In the letter sent to patients after their mammogram.
Notification required: “Your mammogram indicates that you have dense breast tissue. Dense breast tissue is common and is not abnormal. It is found in more than forty percent of women. However, dense breast tissue may make it harder to detect cancer on a mammogram and may also be associated with an increased risk of breast cancer. This information is given to you and your health care provider to raise your awareness of breast density. We encourage you to talk with your health care provider about this and other breast cancer risk factors. Together, you can decide if additional breast imaging would be beneficial based on your mammogram results, risk factors, and physical examination.”
Back To TopTennessee
Effective date: 7/1/2018 (amendment)
Who receives: Patient whose mammogram indicates dense breasts or extremely dense breasts.
How informed: The law states that the facility that performs the mammogram “shall provide” the notification but does not specify how.
Notification required: “Your mammogram shows that you have dense breast tissue. Dense breast tissue is common. However, dense breast tissue can hide breast cancer, so that it may not be seen on routine mammography. It may also be associated with an increased risk of developing breast cancer. You should discuss these results with your doctor to determine if additional tests might be helpful. A report of your mammogram results, which contains information about your breast density, has been sent to your doctor’s office.”
Insurance, effective 8/9/2023: Coverage effective 5/25/22 (see below), shall be provided “…without imposing a deductible, coinsurance, copayment, or a maximum limitation on the application of the deductible, coinsurance, copayment, or other out-of-pocket expense on the patient.”
Insurance, effective 5/25/2022: A health benefit plan that provides coverage for a screening mammogram must provide coverage as follows: A health benefit plan that provides coverage for imaging services for screening mammography must provide coverage to a patient for low-dose mammography according to the following guidelines: (1) A baseline mammogram for a woman thirty-five (35) to forty (40) years of age; (2) A yearly mammogram for a woman thirty-five (35) to forty (40) years of age if the woman is at high risk based upon personal family medical history, dense breast tissue, or additional factors that may increase the individual’s risk of breast cancer; and (3) A yearly mammogram for a woman forty (40) years of age or older based on the recommendation of the woman’s physician. “A health benefit plan that provides coverage for a screening mammogram must provide coverage for diagnostic imaging and supplemental breast screening.” “Supplemental breast screening” means a medically necessary and appropriate examination of the breast, including breast magnetic resonance imaging or breast ultrasound that is: (A) Used to screen for breast cancer when there is no abnormality seen or suspected; and (B) Based on personal family medical history, dense breast tissue, or additional factors that may increase the individual’s risk of breast cancer.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To TopTexas
Effective date: 9/1/2011
Who receives: All patients
How informed: The law does not require or specify that density information be included in the letter sent to patients after their mammogram. The law requires that upon the completion of a mammogram, a mammography facility shall “provide to the patients the following notice.” How the information is provided to the patient is up to the mammography facility.
Notification required: (form of notification up to mammography facility): “If your mammogram demonstrates that you have dense breast tissue, which could hide abnormalities, and you have other risk factors for breast cancer that have been identified, you might benefit from supplemental screening tests that may be suggested by your ordering physician.
Dense breast tissue, in and of itself, is a relatively common condition. Therefore, this information is not provided to cause undue concern, but rather to raise your awareness and to promote discussion with your physician regarding the presence of other risk factors, in addition to dense breast tissue.
A report of your mammography results will be sent to you and your physician. You should contact your physician if you have any questions or concerns regarding this report.”
Insurance, effective 9/1/2021: “A health benefit plan that provides coverage for a screening mammogram must provide coverage for diagnostic imaging that is no less favorable than the coverage for a screening mammogram.” “’Diagnostic imaging’ means an imaging examination using mammography, ultrasound imaging, or magnetic resonance imaging that is designed to evaluate:
(A) a subjective or objective abnormality detected by a physician or patient in a breast;
(B) an abnormality seen by a physician on a screening mammogram;
(C) an abnormality previously identified by a physician as probably benign in a breast for which follow-up imaging is recommended by a physician; or
(D) an individual with a personal history of breast cancer or dense breast tissue.”
Expanded Mammography Coverage, effective 9/1/2017: State law expands definition of “mammography” to include digital mammography or breast tomosynthesis (3D mammograms).
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To Top
Utah
Effective date: 5/8/2018 (amendment). Original 2012 law details below.
Who receives: Patient whose mammogram indicates heterogeneously or extremely dense breasts.
How informed: In the letter sent to patients after their mammogram.
Notification Required: “Your mammogram indicates that you have dense breast tissue. Dense breast tissue is common and is found in as many as half of all women. However, dense breast tissue can make it more difficult to fully and accurately evaluate your mammogram and detect early signs of possible cancer in the breast. This information is being provided to inform and encourage you to discuss your dense breast tissue and other breast cancer risk factors with your health care provider. Together, you can decide what may be best for you. A copy of your mammography report has been sent to your health care provider. Please contact them if you have any questions or concerns about this notice.”
Effective date: 5/8/2012 (original)
Who receives: Undetermined. The law does not require notification but does encourage facilities to provide notice to patients “with dense breast tissue” and to include such notification with the patient’s mammogram results.
The law suggests the following language “may be included”:
“Mammography is the only breast cancer screening examination which has been shown in multiple randomized clinical trials to reduce death rate from breast cancer. However, it is not a perfect test, specifically in women with dense breast tissue. Because your mammogram demonstrates that you have dense breast tissue, you may benefit from supplementary screening tests, depending on your personal risk factors and family history. Although other screening tests may find additional cancers, they may not necessarily increase survival. Nevertheless, you should discuss your mammography results with your health care provider. A copy of your mammography report has been sent to your health care provider’s office. Please contact your health care provider if you have any questions or concerns about this notice.”
Vermont
Effective date: This act shall take effect on July 1, 2016 and shall apply to exams performed on or after January 15, 2017.
Who receives: Every patient must receive information that identifies the patient’s individual breast density classification. Patients with heterogeneously or extremely dense breasts must receive the notification below.
How informed: In the letter sent to patients after their mammogram.
Notification required: The summary of the mammography report shall include a notice substantially similar to the following: “Your mammogram indicates that you have dense breast tissue. Dense breast tissue is a normal finding that is present in about 40 percent of women. Dense breast tissue can make it more difficult to detect cancer on a mammogram and may be associated with a slightly increased risk for breast cancer. This information is provided to raise your awareness of the impact of breast density on cancer detection and to encourage you to discuss this issue, as well as other breast cancer risk factors, with your health care provider as you decide together which screening options may be right for you.”
Insurance, effective 1/1/2019 on such date as a health insurer offers, issues or renews the health insurance plan, but in no event later than 1/1/2020. Insurers shall provide coverage for screening by mammography (including breast tomosynthesis) for the presence of occult breast cancer, as provided by the law’s subchapter. In addition, insurers shall provide coverage for screening by ultrasound for a patient for whom the results of a screening mammogram were inconclusive or who has dense breast tissue, or both. Benefits provided shall cover the full cost of the mammography service or ultrasound, as applicable, and shall not be subject to any co-payment, deductible, coinsurance, or other cost-sharing requirement or additional charge.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To Top
Virginia
Effective date: 7/1/2012, notification language amended to the following effective 7/1/2013
Who receives: Patient whose mammogram indicates heterogeneously or extremely dense breasts.
How informed: In the letter sent to patients after their mammogram.
Notification required: “Your mammogram demonstrates that you have dense breast tissue. Dense breast tissue is very common and is not abnormal. However, dense breast tissue can make it harder to find cancer on a mammogram and may also be associated with an increased risk of breast cancer.
This information is given to you to raise your awareness. Use this information to talk to your doctor about your own risks for breast cancer. At that time, ask your doctor if more screening tests might be useful based on your risk.
A report of your mammography results has been sent to your referring physician’s office, and you should contact your physician if you have any questions or concerns about this report.”
Washington
Effective date: Became law on 6/7/2018, compliance required by 1/1/2019. Law remains in effect through 1/1/2025 unless extended by law.
Who receives: Every patient must receive information that identifies the patient’s individual breast density classification (fatty, scattered, heterogeneously dense or extremely dense). Patients with heterogeneously or extremely dense breasts must receive the notification below.
How informed: In the letter sent to patients after their mammogram.
Notification required: “Your mammogram indicates that you may have dense breast tissue. Roughly half of all women have dense breast tissue which is normal. Dense breast tissue may make it more difficult to evaluate your mammogram. We are sharing this information with you and your health care provider to help raise your awareness of breast density. We encourage you to talk with your health care provider about this and other breast cancer risk factors. Together, you can decide which screening options are right for you.”
Insurance, effective 7/23/2023: “For nongrandfathered health plans issued or renewed on or after January 15 2024, that include coverage of supplemental breast examinations and diagnostic breast examinations, health carriers may not impose cost sharing for such examinations.” “Supplemental breast examination” means a medically necessary and clinically appropriate examination of the breast using breast magnetic resonance imaging or breast ultrasound that is: (a) used to screen for breast cancer when there is no abnormality seen or suspected; and (b) based on personal or family medical history or additional factors that may increase the individual’s risk of breast cancer.
Expanded Mammography Coverage, effective on or about 6/7/2018: State law requires insurers to provide coverage for digital breast tomosynthesis (3D mammograms) with no deductible or cost sharing.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To TopWashington D.C.
Effective date: 3/22/2019
Who receives: Every patient must receive information that identifies the patient’s individual breast density classification (fatty, scattered, heterogeneously dense or extremely dense). Patients with heterogeneously or extremely dense breasts must receive the notification below.
How informed: In the letter sent to patients after their mammogram.
Notification required: “Your mammogram indicates that you have dense breast tissue. Dense breast tissue is relatively common and is not abnormal. Dense breast tissue can, however, make it more difficult to detect cancers in the breast by mammography because it can hide small abnormalities and may be associated with an increased risk for breast cancer. Accordingly, you may benefit from supplementary screening tests, which may include a breast ultrasound screening, or a breast MRI examination, or both, depending on your individual risk factors.
This information is given to you to raise your awareness. Use this information to talk to your health care provider about your own risks for breast cancer. At that time, ask your health care provider if additional screening and/or tests may be useful based on your own risk.
A report of your results was sent to your health care provider. You should contact your health provider if you have any questions or concerns about this report.”
Insurance, effective 3/22/2019: Any individual or group health benefit plan, including Medicaid, shall provide health insurance benefits to cover:
(1) A baseline mammogram for women, including a 3-D mammogram;
(2) An annual screening mammogram for women, including a 3-D mammogram; and
(3) Adjuvant breast cancer screening, including magnetic resonance imaging, ultrasound screening, or molecular breast imaging of the breast, if:
(A) A mammogram demonstrates a Class C or Class D breast density classification; or
(B) A woman is believed to be at an increased risk for cancer due to family history or prior personal history of breast cancer, positive genetic testing, or other indications of an increased risk for cancer as determined by a woman’s physician or advanced practice registered nurse.
Please note, out-of-state, federal, and employer insurance plans set up as “self funded” (check with your benefit administrator) do not, generally, have to comply with state insurance laws. Check with your insurance company regarding details of your coverage.
Back To Top
West Virginia
A bill was introduced in 2023 but did not progress and/or pass into law.
Back To TopWisconsin
Effective date: 4/4/2018
Who receives: Patient whose mammogram indicates heterogeneously or extremely dense breasts.
How informed: In the letter sent to patients after their mammogram.
Notification required: A notice regarding breast density to patients with dense breast tissue in substantially the following form: “Your mammogram shows that your breast tissue is dense. Dense breast tissue is found in almost 40 percent of women and is a normal finding. However, studies show that dense breast tissue can make it harder to find cancer on a mammogram and is associated with a slightly increased risk of breast cancer. Regular screening mammograms are still recommended for you. This information is provided to raise your awareness about the result of your mammogram. You can use this information to talk with your health care professional about your own risks for breast cancer. Together, you can decide which screening options are right for you. The results of your mammogram were sent to your doctor. Please note that breast density is affected by several factors and may change over time.”
Back To TopWyoming
No density notification or insurance legislation has been introduced.
Back To Top