Molecular Breast Imaging (MBI) is a specialized nuclear medicine breast imaging technique that requires intravenous injection of a radiopharmaceutical, typically 99mTc-sestamibi. Sestamibi has been in common use as a tracer for nuclear cardiology studies for over 30 years and has an extremely low risk of adverse reactions and no contraindications. Low-dose molecular breast imaging has been used with excellent results by Mayo Clinic and a few other centers for screening women with dense breasts, showing another 7 to 8 cancers after a normal mammogram for every thousand women screened [1-3].
MBI can also be useful as a diagnostic tool in women who have dense breasts and symptoms such as a lump or vague abnormality on mammography that in rare cases cannot be sorted out with additional views or ultrasound. MBI can also be helpful for some women who need but cannot have an MRI [4]. As of the most recent review in 2017, the American College of Radiology Practice Parameter for Molecular Breast Imaging [5] suggests MBI is a potential option for supplemental screening in high-risk women and those with dense breasts who cannot undergo MRI, but it is usually not indicated, as the technique involves ionizing radiation to the whole body with attendant risk of potentially inducing cancer [6]. MBI is never used in women who are pregnant.
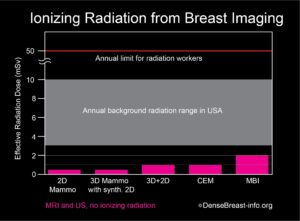
The radiation exposure from low-dose MBI, performed with a delivered dose of 6 to 8 mCi 99mTc-sestamibi, is higher than that from a mammogram. Further, mammography delivers radiation to the breast only, while MBI delivers radiation to the whole body. In order to compare radiation doses from these different types of exams, a standard calculation called “effective radiation dose” is used, which takes into account which body parts are exposed to radiation by a given test and how sensitive every exposed organ is to radiation. Effective dose has units of milli-Sieverts (mSv). The effective dose of mammography is about 0.5 mSv and the effective dose from a low-dose MBI is about 1.8 to 2.4 mSv. For comparison, the radiation dose received from normal daily life is between 3 and 10 mSv per year, depending on where you live [7, 8]. Below effective doses of 100 mSv, no health risks from radiation have been proven according to national and international radiation physics experts [9-11].
Chart 1. This graph shows the whole body effective radiation doses from common breast screening exams: 2D mammography; 3D (tomosynthesis) mammography with synthetic 2D; 2D combined with 3D mammography; contrast-enhanced mammography (CEM); and molecular breast imaging (MBI). MBI, with the highest dose, at 2 mSv, is below the range of annual background radiation exposure in the USA. The annual limit for radiation workers is 50 mSv. At doses below 100 mSv, no risks have been proven, and benefits to patients outweigh any possible risks. Any risk from radiation is greater in younger individuals, especially those under the age of 30, and radiation exposure should always be minimized (except when undergoing cancer treatment).
References Cited
1. Rhodes DJ, Hruska CB, Phillips SW, Whaley DH, O’Connor MK. Dedicated dual-head gamma imaging for breast cancer screening in women with mammographically dense breasts. Radiology2011; 258:106-118
2. Rhodes DJ, Hruska CB, Conners AL, et al. JOURNAL CLUB: Molecular breast imaging at reduced radiation dose for supplemental screening in mammographically dense breasts. AJR Am J Roentgenol2015; 204:241-251
3. Shermis RB, Wilson KD, Doyle MT, et al. Supplemental breast cancer screening with molecular breast imaging for women with dense breast tissue. AJR Am J Roentgenol2016:1-8
4. NCCN Guidelines. Breast cancer screening and diagnosis v.1.2023. National Comprehensive Cancer Network. June 19, 2023. Acessed August 3, 2023. https://www.nccn.org/professionals/physician_gls/pdf/breast-screening.pdf
5. ACR practice parameter for the performance of molecular breast imaging (MBI) using a dedicated gamma camera. American College Of Radiology. Revised 2022. Accessed August 2, 2023. https://www.acr.org/-/media/ACR/Files/Practice-Parameters/MBI.pdf
6. ACR appropriateness criteria: Breast cancer screening. American College Of Radiology. Revised 2017. Accessed August 2, 2023. https://acsearch.acr.org/docs/70910/Narrative/
7. Radiation Sources and Doses. EPA United States Environmental Protection Agency. Updated February 16, 2023. Accessed August 2, 2023. https://www.epa.gov/radiation/radiation-sources-and-doses
8. Biological Effects of Radiation Fact Sheet. United States Nuclear Regulatory Commission. December 2004. Accessed August 2, 2023. https://www.nrc.gov/docs/ML0715/ML071570056.pdf
9. Radiation risk in perspective: Position statement of the Health Physics Society. Health Physics Society. January 1996. Updated February 2019. Accessed August 2, 2023. https://hps.org/documents/radiationrisk.pdf
10. AAPM position statement on radiation risks from medical imaging procedures, Policy number PS 4-A. American Association of Physicists in Medicine. April 10, 2018. Accessed August 2, 2023. https://www.aapm.org/org/policies/details.asp?id=318&type=PP¤t=true
11. Biological Mechanisms of radiation actions at low doses: A white paper to guide the Scientific Committee’s future programme of work. Radiation UNSCotEoA. 2012; Accessed August 2, 2023. https://www.unscear.org/docs/reports/Biological_mechanisms_WP_12-57831.pdf