| QUICK FACTS |
Any additional testing after a mammogram will find more things to be checked. Some may be cancer, but most will not (known as a false positive). To know whether a suspicious finding is cancer or not, further testing and possibly biopsy may be necessary. |
What is it?
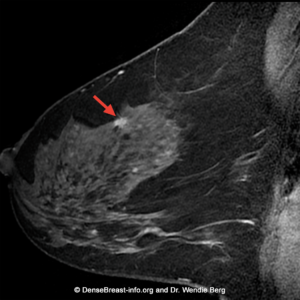
Contrast-enhanced magnetic resonance imaging (MRI) is a medical imaging test that uses very strong magnets and radio waves to create images of the body. Breast MRI requires injection of gadolinium-based contrast agent into a vein in the arm to evaluate the breast tissue (Fig. MRI-1), looking at both anatomy and blood flow patterns. Normal tissue, cancers, and benign (noncancerous) findings can enhance (light up) on MRI. MRI is the most sensitive breast cancer screening modality and is not affected by breast density. MRI is recommended in addition to mammography to screen women at high risk for breast cancer. MRI is also commonly used to assess the local extent of disease to help stage women with newly diagnosed breast cancer. MRI staging is particularly helpful for women with invasive lobular carcinoma (ILC) [1] as it is often underestimated on mammography and ultrasound [2-5].
How it works
For breast MRI, a patient lies face down on a special table with her breasts positioned in an opening called a coil that improves the image quality (Figs. MRI-2, -3). The exam takes place in the “tunnel” of the MRI scanner which makes loud “tapping” noises for several minutes at a time while the imaging is taking place. After an initial set of images has been obtained, a small amount of gadolinium-based contrast agent is injected into a vein in the arm. It is important for the patient to lie still as any motion can reduce image quality and make the images hard to interpret. The usual breast MRI examination takes about 25 minutes.
Abbreviated MRI
A shorter technique, called “abbreviated MRI”, can achieve similar performance when used for screening [6, 7] and may also be offered at some sites. An abbreviated MRI takes fewer images and lasts only about 10 minutes. For individuals with claustrophobia, a sedative can be requested from the referring provider that can be taken 30 minutes prior to the MRI examination. A large multicenter 2020 study [8] compared screening abbreviated MRI to digital breast tomosynthesis in nearly 1500 patients with dense breasts and showed that abbreviated MRI found an additional 9/1000 cancers compared to tomosynthesis (15.2/1000 for abbreviated MRI versus 6.2/1000 for tomosynthesis) in the first year of screening. A smaller, but persistent benefit from adding MRI was identified in the second year as well [9].

Benefits
Even after screening with mammography/tomosynthesis and ultrasound, screening breast MRI reveals an average of 10 additional cancers per thousand women screened (16-17 with the first MRI and 6-7 per year thereafter) [6, 8, 10-13]. The cancer-detection benefit is seen across all breast density categories and for women at average or high risk [10]. MRI detects more cancers than any other screening test and is recommended every year for women who are at high risk for breast cancer, including women with a personal history of breast cancer and dense breasts or diagnosis by age 50 [14]. Many women with dense breasts and a family history of breast cancer or prior biopsy with atypia will meet high-risk criteria (estimated lifetime risk of more than 20%) for screening MRI [15]. For women with dense breasts and no other risk factors who desire supplemental screening, the American College of Radiology recommends MRI [14]. Studies have suggested a slight improvement in cancer detection when MRI is performed on an alternating six-month basis with mammography (e.g. mammogram in January and MRI in July) [16]. There is no benefit to screening US in women having screening MRI [17].
In the DENSE trial in the Netherlands, women with extremely dense breasts and negative mammograms were randomized so that half of them were offered an MRI. In the women who had MRI, there were many fewer symptomatic (interval) cancers that developed between screens and much greater detection of early breast cancer compared to women who had a mammogram alone [12]. As expected, false positives decreased in the second round of MRI screening [13]. These results prompted the European Society of Breast Imaging to recommend screening MRI every 2-4 years among women ages 50-74 with extremely dense breasts [18].
Considerations
Breast MRI will find more areas of concern than either a mammogram or ultrasound. Some of those “finds” will be cancer, but more than half will not (known as a “false positive”). The false positive rate is highest on the first or baseline MRI exam as the radiologist has no prior MRIs for comparison. On subsequent MRIs, the false positive rate decreases. MRIs should be interpreted in conjunction with any other available breast imaging studies, including mammography and ultrasound, as well as knowledge of any prior biopsy results. The facility should also be able to perform an MRI-guided biopsy or have a formal arrangement to refer patients to another facility that has MRI biopsy capability. All facilities accredited in breast MRI by the American College of Radiology should meet these requirements.
MRI cannot be performed in women who have certain metal implants such as a pacemaker or spinal fixation rods. Contrast-enhanced MRI should not be performed if the patient is pregnant. Not all patients can receive gadolinium contrast agent due to allergy or kidney disease. Women with claustrophobia may not be able to tolerate MRI. The positioning can be difficult for some patients with neck problems, obesity or breathing issues. Repeated contrast-enhanced MRIs, including non-breast MRIs, can cause the accumulation of gadolinium in the brain [19], but at this time this is not known to have any harmful effects. There is more accumulation of gadolinium with certain contrast agents that are no longer in widespread use [20].* For women who cannot undergo breast MRI, contrast-enhanced mammography, molecular breast imaging, or possibly ultrasound may be acceptable alternatives if available [14, 21].
For U.S. MRI insurance billing code details, click HERE.
For information about breast imaging insurance laws by state, please visit our Legislation Map HERE.
* “Linear” contrast agents “leak” more gadolinium and therefore show greater accumulation of gadolinium in the brain than “caged” or “macrocyclic” agents. Linear agents include gadopentetate dimeglumine [Magnevist], gadodiamide [Omniscan], and gadoversetamide [OptiMARK]. Macrocyclic agents include gadoterate meglumine [Dotarem], gadobutrol [Gadavist], gadoteridol [ProHance] and gadopiclenol [Vueway].
Latest update: 1/24/24
1. Christensen DM, Shehata MN, Javid SH, Rahbar H, Lam DL. Preoperative breast MRI: Current evidence and patient selection. J Breast Imag 2023;5(2):112-124.
2. Mann RM, Loo CE, Wobbes T, et al. The impact of preoperative breast MRI on the re-excision rate in invasive lobular carcinoma of the breast. Breast Cancer Res Treat 2010;119(2):415-422.
3. Weinstein SP, Orel SG, Heller R, et al. MR imaging of the breast in patients with invasive lobular carcinoma. AJR Am J Roentgenol 2001;176(2):399-406.
4. Fortune-Greeley AK, Wheeler SB, Meyer AM, et al. Preoperative breast MRI and surgical outcomes in elderly women with invasive ductal and lobular carcinoma: a population-based study. Breast Cancer Res Treat 2014;143(1):203-212.
5. Grimm LJ, Johnson KS, Marcom PK, Baker JA, Soo MS. Can Breast Cancer Molecular Subtype Help to Select Patients for Preoperative MR Imaging? Radiology 2014;274(2):352-358.
6. Kuhl CK, Schrading S, Strobel K, Schild HH, Hilgers RD, Bieling HB. Abbreviated breast magnetic resonance imaging (MRI): First postcontrast subtracted images and maximum-intensity projection – A novel approach to breast cancer screening with MRI. J Clin Oncol 2014;32:2304-2310.
7. Mann RM, Kuhl CK, Moy L. Contrast-enhanced MRI for breast cancer screening. J Magn Reson Imaging 2019;50:377-390.
8. Comstock CE, Gatsonis C, Newstead GM, et al. Comparison of abbreviated breast MRI vs digital breast tomosynthesis for breast cancer detection among women with dense breasts undergoing screening. JAMA2020;323:746-756.
9. Kuhl CK. Incidence round screening performance among women with dense breasts undergoing abbreviated breast MRI and digital breast tomosynthesis (ECOG-ACRIN EA1141). J Clin Oncol 41, 2023 (suppl 16; abstr 10502).
10. Kuhl CK, Strobel K, Bieling H, Leutner C, Schild HH, Schrading S. Supplemental breast MR imaging screening of women with average risk of breast cancer. Radiology 2017;283:361-370.
11. Berg WA, Zhang Z, Lehrer D, et al. Detection of breast cancer with addition of annual screening ultrasound or a single screening MRI to mammography in women with elevated breast cancer risk. JAMA. 2012;307(13):1394-1404.
12. Bakker MF, de Lange SV, Pijnappel RM, et al. Supplemental MRI screening for women with extremely dense breast tissue. N Engl J Med 2019;381:2091-2102.
13. Veenhuizen SGA, de Lange SV, Bakker MF, et al. Supplemental Breast MRI for Women with Extremely Dense Breasts: Results of the Second Screening Round of the DENSE Trial. Radiology 2021;299:278-286.
14. Monticciolo DL, Newell MS, Moy L, Lee CS, Destounis SV. Breast Cancer Screening for Women at Higher-than-Average Risk: Updated Recommendations from the ACR. J Am Coll Radiol 2023; published online May 3, 2023.
15. Berg WA, Seitzman RL, Pushkin J. Implementing the national dense breast reporting standard, expanding supplemental screening using current guidelines, and the proposed Find It Early Act. J Breast Imag 2023;5(6):712-723.
16. Lowry KP, Lee JM, Kong CY, et al. Annual screening strategies in BRCA1 and BRCA2 gene mutation carriers: a comparative effectiveness analysis.Cancer2012;118:2021-2030.
17. Berg WA. Data Do Not Support Semiannual Screening US after MRI, and Screening Mammography after MRI Has Limited Benefit. Radiology 2023; 307:e230932, published online May 9, 2023.
18. Mann RM, Athanasiou A, Baltzer PAT, et al. Breast cancer screening in women with extremely dense breasts recommendations of the European Society of Breast Imaging (EUSOBI). Eur Radiol 2022;32:4036-4045.
19. McDonald RJ, McDonald JS, Kallmes DF, et al. Intracranial gadolinium deposition after contrast-enhanced MR Imaging. Radiology 2015;275:772-782.
20. Radbruch A, Weberling LD, Kieslich PJ, et al. Gadolinium retention in the dentate nucleus and globus pallidus is dependent on the class of contrast agent. Radiology 2015;275:783-791.
21. National Comprehensive Cancer Network. NCCN Guidelines. Breast cancer screening and diagnosis v.3.2023. Available at: https://www.nccn.org/professionals/physician_gls/pdf/breast- screening.pdf. Accessed January 23, 2024.
