What Do I Need to Know About Mammograms and Dense Breasts?
1. What is a mammogram? Are there different types of mammograms?
Mammograms are low-dose x-rays that expose the breasts to a small amount of radiation.* Mammograms have been used to screen for breast cancer since the 1980s. There are three different types of mammograms:
- Film: 2-Dimensional, known as “analog” has been nearly eliminated in the U.S.A., but is still in use in Europe and some places in Latin America.
- Digital, 2-Dimensional: known as “Full Field Digital Mammogram” (FFDM). Nearly all facilities in the United States have digital mammography.
- Digital, 3D/tomosynthesis: also referred to as “3-Dimensional” or “tomo.” It is a newer technology that is used in over half of the facilities in the United States is also available in Latin America.
How are a 2D and 3D digital mammogram different?
To explain the difference, think of a 2D mammogram like a photograph of a book. The words on each page of the book would have their letters jumbled on top of the words from all the other pages, so it would be very difficult to read any particular word. Any given “word” could be a small mass due to cancer.
Now, to understand a 3D mammogram, imagine the cover and pages of the book are see-through. The 3D mammogram captures images at different angles, which allows thin “slice” images to be made by the computer. These images can then be viewed one at a time–similar to turning pages of a book and being able to read the words on each page.
A 2D mammogram finds about 5 cancers for every 1,000 women who have a mammogram. Another 1-2 cancers will be found per 1,000 women when 3D/tomosynthesis is used. With 3D mammograms, you are also less likely to be called back for more testing. However, in women with extremely dense breasts, studies have shown mixed results as to whether 3D mammograms find more cancers than 2D mammograms.
*The radiation exposure from a mammogram is small and is too low to cause any harm to the breasts.
To learn more about mammograms, including how they work, benefits and things to consider, click here.
Learn More:
2. Might I have cancer even if my mammogram report is “normal”?
Yes. A “negative,” “benign,” or “normal” mammogram report does not mean cancer is not there. The denser the breast, the more likely it is that a cancer will not show on a mammogram.
| Category of Breast Density | Percent of Cancers That Will Not Show on a Mammogram |
|---|---|
| Extremely dense | 40% |
| Heterogeneously dense | 25% |
| Scattered fibroglandular | 15% |
| Fatty breasts | 10% © DenseBreast-info.org Rev. March 2022 |
Cancer can still be there even if the mammogram report is “normal.” You may want to have an additional screening test after your mammogram to help find cancer. These tests might include one of the following: Ultrasound, MRI, contrast-enhanced mammography or molecular breast imaging (MBI). If your mammogram shows dense breasts, talk with your health care provider about whether you should have an additional screening test after your mammogram.
Learn More:
References
1. Kerlikowske K, Zhu W, Tosteson AN, et al. Identifying women with dense breasts at high risk for interval cancer: a cohort study. Ann Intern Med 2015; 162:673-681
2. Wanders JO, Holland K, Veldhuis WB, et al. Volumetric breast density affects performance of digital screening mammography. Breast Cancer Res Treat 2017; 162:95-103
3. If mammograms miss some cancers in dense breasts, should I still have a mammogram?
Yes. Though both 2D and 3D mammograms can miss cancers in dense breasts, mammograms are still helpful. Some cancers will only be seen on a mammogram (and won’t be seen on Ultrasound or possibly even on MRI).
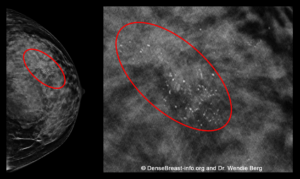
For example, even in dense breasts, mammograms will show calcifications (white specks like salt crystals, see Figure below), which are seen better on mammograms than on Ultrasound. About half of all breast cancers have calcifications. However, most calcifications seen on a mammogram are not due to cancer.
Many studies have shown that finding early stage cancers on a mammogram reduces deaths from breast cancer.
 Mammograms Show About Half of Early Breast Cancers Even in Dense Breasts
Mammograms Show About Half of Early Breast Cancers Even in Dense Breasts
This mammogram of a woman with dense breasts shows a group of calcifications (white specks that are like salt crystals within the red ovals). This patient was diagnosed with invasive breast cancer (“invasive” means it has spread to surrounding breast tissue).
Learn More:
4. I have dense breasts and cancer might be missed on my mammogram, what other screening tests can I do?
5. My recent mammogram was “normal,” but I feel a lump. What should I do?
You should not ignore a lump or any change in your breasts just because your recent mammogram was “normal.” This is especially important if your breasts are dense. While lumps are often cysts or areas of normal tissue, a lump may be cancer that is hidden within dense breast tissue on a mammogram. If you have a lump, you should talk to your health care provider and have a “diagnostic” breast imaging appointment where often an Ultrasound will be performed.
A “normal,” “negative,” or “benign” screening mammogram report does not necessarily mean there is no cancer.
Learn More:
6. Can I just have screening ultrasound and skip mammography?
No. Ultrasound is not a replacement or substitute for mammography. Some breast cancers are only detected by 2D or 3D/tomosynthesis mammography, even in dense breasts.
Learn More:
7. I am a breast cancer survivor and have dense breasts. Is a mammogram enough screening for me?
Maybe not. Women who have had breast cancer are more likely to get a second breast cancer. Some of these cancers are hard to see on a mammogram. In women who have had breast cancer, MRI can help find cancers not seen on a mammogram.
You should talk to your health care provider about having an annual MRI in addition to a 2D/3D mammogram if:
- You were diagnosed with breast cancer by age 50
- You have a history of breast cancer and dense breasts
- You are younger than 70-75
If MRI cannot be performed, ultrasound can be used, but it does not find as many cancers as MRI. If you have a screening MRI, a screening ultrasound is not needed.
A newer breast imaging tool is contrast-enhanced mammography. This may be an option instead of an MRI, but it is not yet widely available. Some centers offer molecular breast imaging (MBI) as an alternative to MRI. Both contrast enhanced mammography and MBI find more cancers than ultrasound. Learn more about screening tests after your mammogram HERE.
If you have had both breasts removed (double mastectomy) and are otherwise in good health, mammograms or other breast imaging tests are not recommended unless there is a lump or other change in the area of surgery or your underarm.
Learn More:
References
1. Monticciolo DL, Newell MS, Moy L, Niell B, Monsees B, Sickles EA. Breast cancer screening in women at higher-than-average risk: Recommendations from the ACR. J Am Coll Radiol 2018; 15:408-414
8. At what age should I start getting mammogram screenings?
Most medical societies in the U.S.A., recommend women begin getting mammograms by age 40.* If you live in Europe, recommendations vary by country; click here to learn more.
The goal of mammogram screenings is to find breast cancer EARLY, when it is easier to treat and most survivable.
Though breast cancer is more common as women get older, it is important to begin mammogram screenings by age 40 because:
- Breast cancer is the number one cause of death in women aged 35 to 54 years.
- Beginning by age 40 lowers the chance of dying from breast cancer.
- Beginning by age 40 is especially important for Asian, Hispanic or Black women as they are more often diagnosed with breast cancer at a younger age.
- More than half of women in their 40s have dense breasts (heterogeneously dense or extremely dense). Dense breasts increase the risk of developing breast cancer and can hide cancer on a mammogram. Women with dense breasts should talk to their health care provider about additional screening after their mammogram.
* Women at “high risk” for breast cancer (for example, those who have a disease-causing genetic mutation such as BRCA1 or BRCA2), should begin getting mammograms even younger – at least by age 30 — and also get an MRI every year.
Learn More:
9. What is a recall and what is a false positive from a mammogram?
About 1 in every 10 women who have a screening mammogram will be called back or “recalled” for extra views or screening tests to look at an area of the breast more closely. THIS IS EXPECTED.
- It is much more common for women to be recalled after their very first mammogram. This is because there is no prior mammogram for comparison to know what is normal for your breasts.
- Among women called back, most (95%) do not have cancer. These are considered false positives or “false alarms.”
Usually, extra mammogram pictures or an ultrasound can clear up a question raised on a mammogram.
About 1 in 5 women called back for additional testing will need a needle biopsy. This is a minor in-office procedure to take a very small sample of breast tissue for testing.
Learn More:
10. Does it matter where I have my mammogram?
Yes. In the United States, a breast imaging center where you get your mammogram must be approved (certified) by the U.S. Food and Drug Administration (FDA). Click here for the list of breast centers approved by the FDA.
An imaging center may receive further certifications through the American College of Radiology (ACR). The ACR’s program designates Breast Imaging Centers of Excellence® based on personnel, policies, equipment, image quality and patient care. Centers of Excellence have ACR certification for stereotactic breast biopsy, ultrasound-guided breast biopsy, and breast MRI. Click here for a list of ACR Breast Imaging Centers of Excellence.
Learn More:

