 Download Comparative Analysis Table
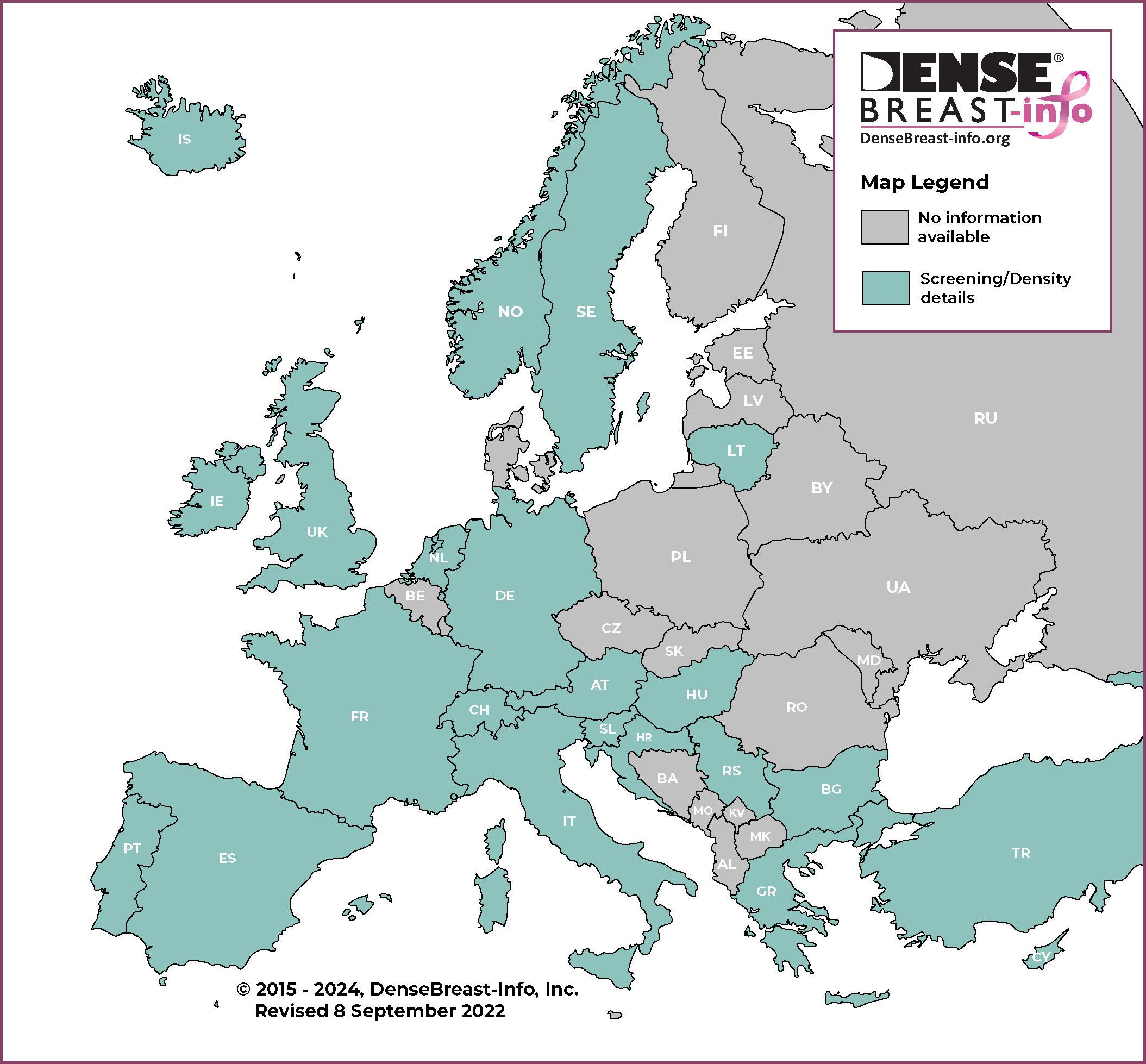
Download Comparative Analysis Table National breast screening programs for women of average risk are offered in nearly all European countries adhering to standards laid out in the European Guidelines for Quality Assurance in Breast Cancer Screening and Diagnosis. These include 2D mammography as the primary screening modality, double reading, centrally collected and evaluated data, technical quality control, and performance targets. Variations do exist on the ages and risk factors of women invited to participate in routine screening, screening intervals, coverage and supplemental screening modalities utilized.
Opportunistic mammography exists in some countries either as the sole screening system or in addition to the national breast screening program. In opportunistic screening, women are advised by their physician or they decide on their own to have a screening mammogram, and programmatic results are not officially monitored. Screening intervals vary depending on many factors (socioeconomic, breast awareness status etc.). Part of the cost is out of pocket payment or reimbursed by private insurance.
Austria
Screening Process:
There is a national (organized) screening program. All equipment is digital and controlled by external quality assurance. Film-screen mammography is not used. All radiologists working in the national screening program must be specifically trained and certified. Breast assessment is performed mainly in specialized hospital departments. Data are collected from all screening and diagnostic mammograms. There is no opportunistic screening.
Recommended age to begin: 45 years (opt-in possible beginning at age 40)
Recommended age to stop: 69 years (opt-in possible at age 69 to continue; no official age to stop)
Recommended screening interval: Every 2 years
Screening Technologies:
National screening program: All sites offer digital mammography and more than 50% offer digital breast tomosynthesis. Supplemental ultrasound is standard in addition to mammography in women with heterogeneously dense or extremely dense breasts.
Opportunistic screening: Not available.
Breast density in medical mammography report: All screening and diagnostic medical mammography reports must include a BI-RADS® density category. No further specific patient notification.
Payment/reimbursement: Free of charge through the national screening program for women between the ages of 45-69 (with opt-in possible at 40 and over age 69).
High-Risk Screening:
Recommended age/modalities/interval: Women with known pathogenic BRCA1 or -2 mutations or equivalent high risk: starting at 18, annual clinical breast exam (CBE); starting at 25, breast MRI; starting at 35, also annual mammogram.
Sources:
http://www.frueh-erkennen.at/
This map content provided by Prof. Michael Fuchsjäger
Reviewed May 2022
Back To TopBulgaria
Screening Process:
No national (organized) screening program – opportunistic screening only. Women are referred by their family doctor or are self-referred. Screening is carried out in primary care facilities.
Recommended age to begin: 50 years
Recommended age to stop: 69 years
Recommended screening interval: Every 2 years
Screening Technologies:
National screening program: Not applicable.
Opportunistic screening: Primary care facilities offer mostly computed radiography (CR) and secondary digitization, some public and private centers offer full-field digital mammography, and a small number of centers still offer film-screen mammography. In public and private facilities tomosynthesis and MRI are available but are not considered on a screening basis. When dense breasts are detected, most radiologists will recommend supplemental ultrasound.
Breast density in medical mammography report: Included in the medical mammography report. BI-RADS® categories are used to describe breast density but are not mandatory.
Payment/reimbursement: Public insurance is available for film-screen and digital mammography. Supplemental ultrasound may be ordered by the family doctor or self-paid.
High-Risk Screening:
Recommended age/modalities/interval: No national guidelines.
Source: Regulation of the Ministry of Health: https://www.nsoplb.com/uploads/docs/_8__03112016_________23112016_.pdf
This map content provided by Dr. Daniela Manolova
Reviewed May 2022
Back To TopCroatia
Screening Process:
There is a national (organized) screening program. Double reading is mandatory.
Recommended age to begin:
National screening program: 50 years
Opportunistic screening: 40 years
Recommended age to stop:
National screening program: 69 years
Opportunistic screening: 75 years; no standard recommendations, according to woman’s preference.
Recommended screening interval:
National screening program: Every 2 years
Opportunistic screening: Annual
Screening Technologies:
National screening program: Public hospitals and county health centers offer digital mammography. For dense breasts, in addition to mammography, supplemental ultrasound is recommended (reimbursed by insurance).
Opportunistic screening: Performed in public or private settings based on woman’s preference/self-referral; includes mammography, ultrasound, digital breast tomosynthesis and MRI.
Breast density in medical mammography report: Included in the medical mammography report for screening mammography. BI-RADS® categories are used to describe breast density. For diagnostic mammography, it is recommended but not required to be included in the report.
Payment/reimbursement: Free of charge through the national screening program. In opportunistic screening, women need to have medical insurance to cover the payment.
High-Risk Screening:
Recommended age/modalities/interval: No national guidelines. Evaluation usually to begin 10 years before the earliest incidence in the family, but not before age 25. Genetic risk counselling is available. Patients are advised and are entitled to further and more frequent screening, referred by their doctor who registers them for mammography/ultrasound or MRI depending on advice received. Women with known pathogenic BRCA1 or -2 mutations or equivalent high-risk: starting at 25; annual breast MRI is recommended with ultrasound recommended six months after the MRI.
Source:
Croatian Guidelines for Quality Assurance in Screening and Diagnosis of Breast Cancer. ISBN 978-953-7031-64-0.
This map content provided by Prof. Boris Brkljačić
Reviewed April 2022
Back To TopCyprus
Screening Process:
National Health Service (organized) screening program. In opportunistic screening, women are referred by their family doctor.
Recommended age to begin:
National screening program: 45 years
Opportunistic screening: 40 years and baseline mammography at 35 years.
Recommended age to stop:
National screening program: 74 years
Opportunistic screening: Until life expectancy is less than 5 years.
Recommended screening interval:
National screening program: Every 2 years. If breasts are heterogeneously dense or extremely dense, every year.
Opportunistic screening: Every 1-2 years; depending on risk factors; usually every 1-1.5 years from age 40-75 and every 2 years after age 75.
Screening Technologies:
National screening program: Digital mammography; if breasts are heterogeneously dense or extremely dense, ultrasound beginning 6 months after the screening mammogram and continuing annually.
Opportunistic screening: Digital mammography, may be complemented by tomosynthesis in some centers. In women with dense breasts, ultrasound is recommended annually or at six-month intervals, alternating with mammography.
Breast density in medical mammography report: In the national screening program, BI-RADS® density is included in the medical mammography report if the patient has heterogeneously or extremely dense breasts.
In opportunistic screening, BI-RADS® density is included in the medical mammography report for all women.
Payment/reimbursement: Free of charge through the national screening program. In opportunistic screening, women need to pay or have medical insurance to cover the payment.
High-Risk Screening:
No national guidelines. In the private sector, based on family history, women are referred by medical practitioners, gynecologists or oncologists and screened with digital breast tomosynthesis. Women with known pathogenic BRCA1 or -2 mutations or equivalent high-risk: annual MRI is recommended in addition to mammography.
Sources:
Government and Parliament site/Cyprus Ministry of Health:
https://www.moh.gov.cy/moh/moh.nsf/index_gr/index_gr?OpenDocument
Cyprus Radiological Society:
https://cyradiology.com
This map content provided by Dr. Chrysa Tziakouri-Shiakalli
Reviewed April 2023
Back To TopFrance
Screening Process:
A national (organized) screening program. Non-high-risk women are invited to participate by mail. Approved radiologists interpret screening examinations. A second reader reviews normal screening mammograms. In cases with abnormal findings, the first reader performs immediate diagnostic work-up. There is also opportunistic screening where patients are referred by their gynecologist or family doctor.
Recommended age to begin:
National screening program: 50 years
Opportunistic screening: No standard recommendations, usually 40 years; according to referring doctor.
Recommended age to stop:
National screening program: 74 years
Opportunistic screening: No standard recommendations, according to referring doctor.
Recommended screening interval:
National screening program: Every 2 years
Opportunistic screening: Every 1 to 2 years
Screening Technologies:
National screening program: Film-screen or digital mammography and ultrasound; supplemental ultrasound is recommended in women with heterogeneously dense and extremely dense breasts. Digital breast tomosynthesis for diagnostic work-up.
Opportunistic screening: Digital breast tomosynthesis is used routinely in both screening and diagnostic setting.
Breast density in medical mammography report: Included in the medical mammography report. BI-RADS® categories are used to describe breast density.
Payment/reimbursement: In the national screening program, bilateral mammography is free of charge for the patient. Cost of additional ultrasound is charged to the patient and is most often partly or totally reimbursed by national or personal health insurance.
High-Risk Screening:
Recommended age/modalities/interval: Women with known pathogenic BRCA1 or -2 mutations or equivalent high-risk: starting at 30, annual MRI followed by one view (MLO) bilateral mammography and, in women with dense breasts, ultrasound is offered.
Sources:
http://www.e-cancer.fr/Professionnels-de-sante/Depistage-et-detection-precoce/Depistage-du-cancer-du-sein/Le-programme-de-depistage-organise
http://www.e-cancer.fr/Actualites-et-evenements/Actualites/Femmes-porteuses-d-une-mutation-de-BRCA1-ou-de-BRCA2-l-Institut-actualise-ses-recommandations
This map content provided by Prof. Isabelle Thomassin-Naggara; Dr Foucauld Chamming’s
Reviewed June 2022
Back To TopGermany
Screening Process:
A national screening (organized) program. In opportunistic screening, women are referred by their gynecologist, primary care provider, breast surgeon or are self-referred.
Recommended age to begin:
National screening program: 50 years
Opportunistic screening: 40 years
Recommended age to stop:
National screening program: 69 years
Opportunistic screening: 80+ years according to individual policy and woman’s preference.
Recommended screening interval:
National screening program: Every 2 years
Opportunistic screening: Every 1-2 years, with individual appointments by the woman.
Screening Technologies:
National screening program: Public units offer digital mammography. Digital breast tomosynthesis, ultrasound or MRI is only used for diagnostic assessment, not for screening.
Opportunistic screening: Digital mammography, ultrasound, MRI, digital breast tomosynthesis. No formal guidelines.
Breast density in medical mammography report: In the national screening program, no guidelines for density notification. In opportunistic screening, density information is included in every medical mammography report. Most gynecologists and radiologists will explain the issue and suggest supplemental ultrasound or much less often, but with increasing frequency, MRI, in women with dense breasts. BI-RADS® categories are used to describe breast density.
Payment/reimbursement: Public insurance for biennial screening mammography ages 50-69; in women ages 40-49, opportunistic mammographic screening is discouraged by public insurance companies and thus not reimbursed in women with public insurance; in women with private insurance, this is variable. Private insurance usually covers supplemental screening ultrasound in women with dense breasts.
High-Risk Screening:
Recommended age/modalities/interval: For women with known pathogenic BRCA1 or -2 mutation or equivalent high-risk: annual MRI and ultrasound until age 40, thereafter annual MRI and annual mammography as well as ultrasound at six-month intervals. Age to start depends on the age of the youngest family member but age 30 at the latest
Sources:
http://www.mammo-programm.de/
This map content provided by Prof. Alexander Mundinger; Prof. Christiane Kuhl
Reviewed November 2022
Back To TopGreece
Screening Process:
There is a national (organized) screening program. In opportunistic screening, women are referred by their gynecologist, primary care provider, breast surgeon or are self-referred.
Recommended age to begin:
National screening program: 50 years
Opportunistic screening: 40 years
Recommended age to stop:
National screening program: 69 years
Opportunistic screening: 72 years (continue every 2 years if the woman is in good health with >5-7 years life expectancy)
Recommended screening interval:
National screening program: Every 2 years
Opportunistic screening: Annual
Screening Technologies:
National screening program: Film-screen or digital mammography and ultrasound. In most hospitals, there is a computer radiography option. In some hospitals, digital breast tomosynthesis is available. Supplemental breast ultrasound is recommended (but not mandatory) for heterogeneously dense and extremely dense breasts.
Opportunistic screening: Public hospitals offer film-screen, digital mammography, digital breast tomosynthesis, ultrasound and breast MRI. Private sector offers digital mammography, digital breast tomosynthesis, ultrasound, automated breast ultrasound and MRI. In most centers, supplemental ultrasound is offered to women with dense breasts.
Breast density in medical mammography report: Included in the medical mammography report. BI-RADS® categories are used to describe breast density.
Payment/reimbursement: Public insurance for film-screen or digital mammography and supplemental breast ultrasound. In private centers under contract with public providers, women need to co-finance 15%.
High-Risk Screening:
Recommended age/modalities/interval: Evaluation to begin 5-10 years before the earliest incidence in family. Women with known pathogenic BRCA1 or -2 mutations or equivalent high-risk: under age 25, clinical breast exam (CBE) and ultrasound; starting at 25, annual MRI and ultrasound at six-month intervals; starting at 35, add annual mammography.
Source:
National Society of Breast Imaging guidelines: http://www.hbis.gr/
This map content provided by Dr. Athina Vourtsis
Reviewed January 2023
Back To TopHungary
Screening process:
There is a national organized screening program for average-risk women aged 45–65. Both digital mammography and film-screen mammography are available. Trained and certified radiologists are working in the national screening program. A second reading is applied. Breast assessment is performed in specialized hospital departments and diagnostic centres (outpatient clinics). Data are collected from all screening and diagnostic mammograms in the national health insurance database. For opportunistic screening, women are referred by their primary care provider or gynaecologist.
Recommended age to begin:
National screening program: 45 years (opt-in possible at age 40)
Opportunistic screening: 40 years (average risk)
Recommended age to stop:
National screening program: 65 years (opt in possible beyond age 65)
Opportunistic screening: No standard recommendation
Recommended screening interval:
National screening program: Every 2 years
Opportunistic screening: Every 1-2 years (depending on risk factors)
Screening technologies:
National screening program: All sites offer both digital mammography and film-screen mammography. Supplemental ultrasound is routinely performed in addition to mammography in women with heterogeneously dense or extremely dense breasts.
Opportunistic screening: Digital mammography. Digital breast tomosynthesis is available, but not routinely used in either the screening or diagnostic setting.
Breast density in medical mammography report: Screening and diagnostic medical mammography reports must include a BI-RADS® density category. No further specific patient notification.
Payment/reimbursement: Free of charge through the national screening program for women aged 45–65.
High-risk screening:
Recommended age/modalities/interval: For women with known pathogenic BRCA1 or BRCA2 mutations or equivalent, high-risk screening is suggested to begin at age 30 with annual mammography/ultrasound combined as the standard modality; MRI is also recommended for supplemental screening if available. The same algorithm is valid for high-risk women carrying a TP53 mutation, from age 20. Genetic risk counselling is available.
Sources:
https://onkol.hu/wp-content/uploads/2020/06/radiol%C3%B3gia.pdf
This map content provided by Prof. Ádám László; Dr. Dora Bokor
Reviewed April 2022
Back To TopIceland
Screening Process:
A national (organized) screening program is run by the Icelandic Cancer Society (ICS) and under the surveillance and licence of the Icelandic Ministry of Health. Double reading interpretation is performed. Opportunistic screening is infrequent. Women are referred by their general practitioner, gynecologist, breast surgeon, etc. for diagnostic assessment.
Recommended age to begin:
National screening program: 40 years
Opportunistic screening: No recommendation
Recommended age to stop:
National screening program: 69 years; women 70 and over can self-refer.
Opportunistic screening: No recommendation
Recommended screening interval:
National screening program: Every 2 years
Opportunistic screening: No recommendation
Screening Technologies:
National screening program: 2D digital mammography.
Opportunistic screening: 2D digital mammography.
No additional screening is offered to women with dense breasts.
Breast density in medical mammography report: Breast density is not routinely included in the medical mammography report and there are no guidelines for density notification. BI-RADS® density categories are not generally used.
Payment/reimbursement: The screening fee in the national screening system is paid for by the participating individual.
High-Risk Screening:
Recommended age/modalities/interval: Women with family history: mammogram and MRI 5 years before earliest incidence in the family. Women with known pathogenic BRCA1 or -2 mutations or equivalent high-risk: age 25-74, annual mammogram; age 25-55, include annual MRI.
Sources:
https://www.krabb.is/english.
This map content provided by Dr. Magnús A. Lúðvíksson
Back To TopIreland (Republic of)
Screening Process:
A national (organised) screening program, BreastCheck. In opportunistic screening, women are referred by their family doctor, gynecologist, primary care provider or are self-referred. National screening program takes place in 4 dedicated static screening centres (2 in the east, 1 in the south and 1 in the west), each supported by dedicated mobile units.
Recommended age to begin:
National screening program: 50 years
Opportunistic screening: No standard minimum age; generally through private hospital breast clinics or in public hospital setting as justified by referral based on family history, previous history of cancer.
Recommended age to stop:
National screening program: 69 years
Opportunistic screening: No standard recommendations; according to woman’s preference.
Recommended screening interval:
National screening program: Every 2 years
Opportunistic screening: Every 1-2 years or as per referring doctor’s request.
Screening Technologies:
National screening program: Digital mammography and ultrasound. Digital breast tomosynthesis is available in all static screening units and is primarily used for assessment clinics. No distinct guidelines for women with dense breasts.
Opportunistic screening: Public/private hospitals do not offer screening as part of the national screening program. Private sector offers film-screen or digital mammography and ultrasound.
Breast density in medical mammography report: Not routinely recorded and not included in the mammography report. In the assessment service, individual radiologists include a statement referring to breast density, but do not use BI-RADS® categories.
Payment/reimbursement: No cost to patient in a public hospital, or as part of the breast screening service. In private centres, screening is at cost to the patient with some potential reimbursement depending on medical insurance.
High-Risk Screening:
Recommended age/modalities/interval: No specific national guidelines. Department/hospital specific and include MRI.
This map content provided by Éilish McDermott; Mairead Crowley; Dr. Jonathan McNulty
Reviewed May 2022
Back To TopItaly
Screening Process:
There is a national screening (organized) program. In opportunistic screening, women are referred by their gynecologist, primary care provider, breast surgeon or are self-referred.
Recommended age to begin:
National screening program: 50 years; each Italian region decides independently whether to extend and finance invitation to start at age 45
Opportunistic screening: 40 years with baseline mammogram between 35-40, depending on family history
Recommended age to stop:
National screening program: 69 years (70-74 under study); each Italian region decides independently whether to extend and finance invitation to continue to age 74
Opportunistic screening: No standard recommendations; according to woman’s preference.
Recommended screening interval:
National screening program: Every 2 years (every 12-18 months between 40-49)
Opportunistic screening: Variable: Every 1 – 2 years
Screening Technologies:
National screening program: Digital mammography; digital breast tomosynthesis (available in 2 of 20 regions).
Opportunistic screening: Digital mammography, digital breast tomosynthesis and ultrasound for women with dense breasts.
Breast density in medical mammography report:
National screening program: No national guidelines.
Opportunistic screening: When density is reported, BI-RADS® categories are used.
Payment/reimbursement: Free of charge through the national screening program. In opportunistic screening, cost of additional screening (beyond that offered in the national program) is charged to the patient and women may have medical insurance to cover the payment. There is an exemption for payment in some regions for women with a personal history of breast cancer or based on inability to pay.
High-Risk Screening:
Recommended age/modalities/interval: Women with known pathogenic BRCA1 or -2 mutations or equivalent high-risk: starting age 25, annual MRI; starting age 30, annual mammography (if MRI not available); starting age 30, annual ultrasound (if MRI not available). Guidelines for high-risk differ in each region. High-risk screening is billed to the patient or women may have medical insurance to cover the payment.
Sources:
https://www.osservatorionazionalescreening.it/
http://www.gisma.it/
http://www.registri-tumori.it/cms/
This map content provided by Prof. Enzo Durante; Dr. Adriana Bonifacino
Reviewed January 2023
Back To TopLithuania
Screening Process:
No national (organized) screening program – opportunistic screening only. Women are referred by their family doctor or gynecologist or can be self-referred. Primary care institutions and family doctors receive financial support from the National Health Insurance fund for every woman referred to screening.
Recommended age to begin: 50 years
Recommended age to stop: 69 years
Recommended screening interval: Every 2 years
Screening Technologies:
National screening program: Not applicable
Opportunistic screening: Medical institutions participating in screening offer film-screen or digital (CR or DR) mammography; rarely tomosynthesis. Generally, supplemental ultrasound is offered to women only after positive mammography report and with a referral from a specialist. Supplemental ultrasound is often recommended if the breasts are dense. In women with extremely dense breasts, MRI is reimbursed by public insurance after specialist referral.
Breast density in medical mammography report: Breast density is included in the medical mammography report using four categories, similar to BI-RADS®.
Payment/reimbursement: Public insurance for mammography; ultrasound or MRI if recommended by a radiologist. No cost to patients if center is under contract with public providers.
High-Risk Screening:
Recommended age/modalities/interval: No population screening; mammogram 5-10 years before the earliest incidence in family. Women with known pathogenic BRCA1 or -2 mutations or equivalent high-risk are recommended to start clinical breast exam (CBE) starting at age 25, annual MRI and ultrasound at six-month intervals starting at age 25 and annual mammography starting at age 35-40. Public insurance covers breast MRI in cases of known pathogenic BRCA or other mutations associated with breast cancer.
Sources: No screening guidelines; Ministry of Health order about funding of screening program.
https://www.esavadai.lt/dokumentai/1530-lr-sam-isakymas-del-atrankines-mamografines-patikros-del-kruties-vezio-finansavimo-programos-patvirtinimo-pakeitimai-nuo-2017-07-01/.
This map content provided by Dr. Rūta Briedienė
Reviewed May 2022
Back To TopThe Netherlands
Screening Process:
The Dutch government, the Ministry of Health, Welfare and Sport, is the commissioning party for the Bevolkingsonderzoek borstkanker (Population-based breast screening programme). On behalf of the Ministry, the RIVM (National Institute for Health and Environment) coordinates and directs the screening programme. Five screening organizations coordinate the execution regionally in a uniform way. Quality assurance of the breast cancer screening initiative is carried out by the LRCB (National Reference Center for Breast Cancer). Additionally, a National Evaluation Team Breast Cancer yearly evaluates the execution, impact and costs of the screening program to allow for possible adjustments. In opportunistic “screening”, women are referred by their primary care provider because of symptoms.
Recommended age to begin:
National screening program: 50 years
Opportunistic screening: No standard recommendation
Recommended age to stop:
National screening program: 75 years
Opportunistic screening: No standard recommendation
Recommended screening interval:
National screening program: Every 2 years.
Opportunistic screening: No standard recommendation
Screening Technologies:
National screening program: Standard digital mammography. No additional screening is offered to women with dense breasts.
Opportunistic screening: No standard recommendation
Breast density in medical mammography report: Not included in the medical mammography report in the national screening program. When density is reported (in diagnostic breast imaging), BI-RADS® categories are used.
Payment/reimbursement: The screening program is paid for by the government; diagnostic follow-up assessments are not included and fall under the (mandatory) national health insurance system. In opportunistic screening, all costs fall under the national health insurance system (depending on the deductible amount of the insurance claim the woman has chosen, she has to pay for the opportunistic screening herself or it is covered by the insurance).
High-Risk Screening:
Recommended age/modalities/interval: Eligibility for high-risk screening is determined according to a detailed diagram using patient age, high-risk genes, and history of breast/ovary/tubal cancer of the woman and in the family. Women with a known pathogenic BRCA1 mutation receive yearly MRI from ages 25-60, and bi-annual mammography between the ages of 40-75 (i.e. partially overlapping with the MRI imaging); if such women have dense breasts, they receive alternating MRI and mammography every six months between the ages of 60-75.
Sources:
https://www.oncoline.nl/richtlijn/item/index.php?pagina=/richtlijn/item/pagina.php&richtlijn_id=1097
https://www.rivm.nl/bevolkingsonderzoek-borstkanker/.
Norway
Screening Process:
In BreastScreen Norway, the four regional health authorities offer mammographic screening through 17 breast centres and associated screening units. In opportunistic screening, women are referred by their gynecologist, primary care provider, breast surgeon or are self-referred.
Recommended age to begin:
National screening program: 50 years
Opportunistic screening: No recommendation.
Recommended age to stop:
National screening program: 69 years
Opportunistic screening: No recommendation.
Recommended screening interval:
National screening program: Every 2 years
Opportunistic screening: No recommendation
Screening Technologies:
National screening program: Standard digital mammography
Opportunistic screening: Standard digital mammography
Breast density in medical mammography report: Not a part of the medical mammography report in the national screening program.
Payment/reimbursement: Women pay their local health trust a fee of NOK 267 for screening in BreastScreen Norway. For further assessment women pay an additional deductible.
In opportunistic screening, the woman pays the usual deductible (NOK 267) if she obtains mammography at a private clinic that is covered via the national health insurance system. Otherwise, the fee is higher, and varies by individual hospital/clinic.
High-Risk Screening:
Recommended age/modalities/interval: Women with known pathogenic BRCA1 or -2 mutations or equivalent high-risk: starting at 25, annual mammogram and MRI.
Sources:
https://www.kreftregisteret.no/en/screening/BreastScreen_Norway/breastscreen-norway/
Reviewed May 2022
Back To TopPortugal
Screening Process:
A national (organized) screening program takes place at dedicated fixed or mobile screening units. Women of screening age are selected from national health service users list and invited to participate. In opportunistic screening, women are referred to private practices by their gynecologist or family doctor.
Recommended age to begin:
National screening program: 50 years (Mainland Portugal); 45 years (Archipelagos of Madeira and Azores)
Opportunistic screening: Usually 40-45 years
Recommended age to stop:
National screening program: 69 years (Mainland Portugal and Archipelago of Madeira); 74 years (Archipelago of Azores)
Opportunistic screening: No standard recommendations; according to women’s preference and doctor’s referral.
Recommended screening interval:
National screening program: Every 2 years
Opportunistic screening: Variable: Every 1-2 years.
Screening Technologies:
National screening program: Mainland Portugal and Archipelago of Azores – Digital mammography (DM) (double reading; centrally collected and evaluated data, technical quality control according to standards laid out in the European Guidelines for Quality Assurance in Breast Cancer Screening and Diagnosis); Archipelago of Madeira – DM (double reading); Algarve Region – DM with Digital Breast Tomosynthesis (DBT).
Opportunistic screening: Variable. Mostly DM with ultrasound (independent of breast density); some centers offer DBT with different protocols; MRI more often available for women with dense breasts. No specific indication for supplemental screening in dense breasts but MRI or ultrasound often performed.
Breast density in medical mammography report: Variable. Breast density is included in most medical mammography reports. BI-RADS® categories are used to describe breast density.
Payment/reimbursement: Free of charge through the national screening program. In opportunistic screening, costs are charged to the patient and most often partly or totally reimbursed by national health system funds or personal health insurance.
High-Risk Screening: Recommended age/modalities/interval:
Screening of healthy BRCA1 and BRCA2 mutation carriers: Clinical examination and imaging starting 5 to 10 years before the age at diagnosis of the youngest family member with breast cancer, being mandatory after 25 years old; annual screening with MRI and, after age 30, also DM.
Screening of healthy non-BRCA mutation carriers: PTEN – annual MRI starting at 30-35 years or 5 to 10 years before the age at diagnosis of the youngest family member with breast cancer; personalized screening after 75 years; ATM, CHEK 2, NBN – annual MRI starting at 40 years; PALB2 – annual MRI from 30 to 69 years; CDH1 – annual MRI starting at 30 years; NF1 – annual MRI from 30 to 50 years, DM when risk equals that of general population; TP53 – annual MRI starting from 20 (earlier if younger family members with breast cancer) to 75 years.
Screening of high-risk women without known mutations (Gail >1.7% 5-year risk; IBIS > 20% lifetime risk): Imaging starting between 25 years and 5 to 10 years before the age at diagnosis of the youngest family member with breast cancer, mandatory after 25 years; annual screening with DM and MRI.
Sources:
https://www.ligacontracancro.pt/servicos/detalhe/url/programa-de-rastreio-de-cancro-da-mama/
https://portal.azores.gov.pt/web/coa/rocma
This map content provided by Dr. Mónica Armas
Reviewed May 2022
Back To TopSerbia
Screening Process:
A national (organized) screening program. In opportunistic screening, women are referred by their family doctor or gynecologist. National screening program takes place in public hospitals and public primary care facilities.
Recommended age to begin:
National screening program: 50 years
Opportunistic screening: 30+ years, ultrasound every 1-2 years; age 40 years, mammography every 2 years; ultrasound in alternating years.
Recommended age to stop:
National screening program: 69 years
Opportunistic screening: No standard recommendations; according to woman’s preference.
Recommended screening interval:
National screening program: Every 2 years
Opportunistic screening: Every 1-2 years
Screening Technologies:
National screening program: Film-screen or digital mammography and ultrasound. In most hospitals, there is a computed radiography option for secondary digitization. In some hospitals, digital breast tomosynthesis is available. Supplemental ultrasound is recommended but not mandatory for heterogeneously dense and extremely dense breasts.
Opportunistic screening: Private hospitals do not offer national screening. Private sector offers film-screen or digital mammography and ultrasound. Several private institutions offer digital tomosynthesis and breast MRI.
Breast density in medical mammography report: Included in the medical mammography report. BI-RADS® categories are used to describe breast density.
Payment/reimbursement: Public insurance is available for film-screen and digital mammography, as well as for ultrasound, tomosynthesis and breast MRI. In private centers, screening is at cost to the patient with no reimbursement.
High-Risk Screening:
Recommended age/modalities/interval: No national guidelines. Evaluation to begin 5-10 years before the earliest incidence in the family. Women with known pathogenic BRCA1 or -2 mutations or equivalent high-risk: under age 25 and until age 40, ultrasound; starting at 40, annual mammogram and MRI.
Source:
http://www.skriningsrbija.rs/eng/breast-cancer-screening
This map content provided by Prof. Dragana Djilas
Reviewed September 2022
Back To TopSlovenia
Screening Process:
A national (organized) screening program. National screening program takes place in public hospitals, public primary care facilities and mobile units. In opportunistic screening, women are referred by their family doctor, gynecologist, primary care provider or are self-referred.
Recommended age to begin:
National screening program: 50 years
Opportunistic screening: No standard recommendations, according to woman’s preference.
Recommended age to stop:
National screening program: 69 years
Opportunistic screening: No standard recommendations, according to woman’s preference.
Recommended screening interval:
National screening program: Every 2 years
Opportunistic screening: No standard recommendations, according to woman’s preference.
Screening Technologies:
National screening program: Digital mammography. In some hospitals, digital breast tomosynthesis is available. No additional screening is offered to women with dense breasts.
Opportunistic screening: Private hospitals do not participate in national screening. Private sector offers digital mammography, ultrasound and breast MRI.
Breast density in medical mammography report: Breast density will soon be included in the medical mammography reports in the national screening program, using BI-RADS® categories to describe breast density.
Payment/reimbursement: Public insurance covers digital mammography, ultrasound, tomosynthesis and breast MRI in public breast centers. In private centers all examinations are paid by the patient or private insurance with no reimbursement from public health insurance company.
High-Risk Screening:
Recommended age/modalities/interval: For women with known pathogenic BRCA1 or BRCA2 mutations or equivalent, high-risk screening is suggested to begin at age 25 or earlier with annual MRI and ultrasound until the age of 30 and thereafter annual mammography and MRI.
This protocol is also used for women with a family history of breast cancer diagnosed before age 30. For high-risk women carrying a TP53 mutation, annual MRI and ultrasound are recommended to start at age 20 with annual mammography and MRI beyond age 30. Genetic risk counselling is available.
Source:
https://dora.onko-i.si/english
This map content provided by Dr. Janja Škerjanec
Reviewed August 2022
Back To TopSpain
Screening Process:
A national (organized) screening program, performed in public hospitals. In opportunistic screening, women are referred by their gynecologist, primary care provider, breast surgeon or are self-referred.
Recommended age to begin:
National screening program: 50 years
Opportunistic screening: 40 years
Recommended age to stop:
National screening program: 69 years
Opportunistic screening: No standard recommendations; according to woman’s preference.
Recommended screening interval:
National screening program: Every 2 years
Opportunistic screening: Annual
Screening Technologies:
National screening program: Digital mammography and ultrasound. Supplemental ultrasound is recommended but not mandatory for heterogeneously dense and extremely dense breasts. Some hospitals are beginning to use tomosynthesis.
Opportunistic screening: Digital mammography, digital breast tomosynthesis, ultrasound, automated breast ultrasound and MRI. At the discretion of the radiologist/center, ultrasound may be performed in women with dense breasts. Some private medical centers recommend 3D ultrasound for asymptomatic women with dense breasts.
Breast density in medical mammography report: Not mandatory in the medical mammography report in the national screening program. Electively, BI-RADS® categories are used to describe breast density in opportunistic screening.
Payment/reimbursement: Public insurance for film-screen and digital mammography. In opportunistic screening, women need to have medical insurance to cover the payment; normally private medical insurance covers 100% of payment.
High-Risk Screening:
Recommended age/modalities/interval: Women with known pathogenic BRCA1 or -2 mutations or equivalent high-risk: starting at 25, annual mammogram and MRI and ultrasound at alternating six-month intervals.
Source:
http://www.sedim.org/nueva/wp-content/uploads/2014/10/Programa_Garant%C3%ADa_Calidad_SEDIM.pdf
This map content provided by Dr. Francisca Gras Canals
Reviewed May 2022
Back To TopSweden
Screening Process:
There is a national (organized) screening program. The Swedish National Health Board provides breast screening to the Swedish counties, by invitation, with mammography at no cost. The screening program is non-obligatory; rather, it is strongly recommended to all women from age 40-74. The same service is offered at no cost to the patient in public hospitals or through private mammography clinics, paid by the counties. Opportunistic screening in private clinics is also offered throughout the country, where women are referred mainly by general practitioners or by their gynecologists.
Recommended age to begin:
National screening program: 40 years
Opportunistic screening: Any age. For women 26 years and younger, ultrasound. In case of pathology, further workup with mammography/MRI if required. For women older than 26 years, mammography; further pathology workup as needed.
Recommended age to stop:
National screening program: 74 years
Opportunistic screening: At any age
Recommended screening interval:
National screening program: 18-24 months in age groups 40-74
Opportunistic screening: Individualized
Screening Technologies:
National screening program: Digital mammography only. No additional screening is offered to women with dense breasts.
Breast density in medical mammography report: No national guidelines. Breast density is included in the mammography reports at the radiologist’s discretion. BI-RADS® breast density classification system is most commonly used, with some use of Tabár system.
Payment/reimbursement: Free of charge
High-Risk Screening:
Recommended age/modalities/interval: Women with pathogenic BRCA1 or -2 mutations are offered screening starting at age 25 up to age 30 with MRI and ultrasound, alternating at six-month intervals. Those women older than 30 are offered MRI, followed by ultrasound and mammography annually. For other women at high risk (personal history of breast cancer, chest radiation therapy prior to age 30, etc.) a personalized decision is made (which may include annual MRI and/or mammography and ultrasound) by breast surgeons and oncologists. For breast cancer survivors, annual mammography and in some cases ultrasound is offered for 5 years after the patient has completed treatment.
Source:
Sweden-14mar2013_delegate_workshop_karin leifland.pdf
This map content provided by Dr. Fofi Kakoulidis
Back To TopSwitzerland
Screening Process:
There are national quality standards, though there is no national organized screening program. Several regional organized screening programs exist, mainly in the French speaking regions, covering about half the country; mammograms offered in public and private radiologic centers. Well-developed opportunistic screening, with women referred in public and private radiologic centers by their gynecologist or family doctor.
Recommended age to begin:
Regional screening program: 50 years
Opportunistic screening: No standard recommendation, usually 40-50 years according to the referring doctor
Recommended age to stop:
Regional screening program: 74 years
Opportunistic screening: No standard recommendation, (usually over age 80, according to woman and/or referring doctor preference)
Recommended screening interval
Regional screening program: Every 2 years
Opportunistic screening: Every 1 -2 years, according to woman and/or referring doctor preference
Screening Technologies:
Regional screening program: digital mammography; since 2016, recommendation of adding ultrasound in women with dense breasts (most centers).
Opportunistic screening: digital mammography, ultrasound, MRI
Additional ultrasound in women with dense breasts (most centers).
Breast density in medical mammography report: Regional screening program: BI-RADS® density included in the medical mammography report.
In opportunistic screening BI-RADS® density not routinely included (varies by individual radiologist).
Payment/reimbursement: Regional screening program: 10% of the cost of the mammogram is charged to the patient. If the patient has dense breasts, there is an additional cost for US which is partially reimbursed (usually 90%, depending on the type of insurance contract). Opportunistic screening: charged to the woman, but reimbursed partially, usually 90%, according to the type of insurance contract.
High-Risk Screening:
Recommended age/modalities/interval: Women with mother/sister/daughter with history of breast cancer or >30% life-time risk, up to one mammogram per year beginning at age 30 (and additional screening ultrasound if dense breast); after age 60, every two years.
Women with known pathogenic BRCA1 or 2-mutations or p53 mutations: annual MRI and mammography with ultrasound at alternating six-month intervals.
Sources:
Swiss Society of Senology: https://www.senologie.ch/fr/info-du-sein/opas/
Swiss cantons with current breast cancer screening program in 2022 (pdf): https://www.swisscancerscreening.ch/fr/offres-dans-votre-canton
This map content provided by Dr. Dominique Fournier
Reviewed June 2022
Back To TopTurkey
Screening Process:
A national (organized) screening program, performed in screening centers and mobile mammography units. In opportunistic screening, women are referred by their gynecologist, primary care provider, breast surgeon or are self-referred.
Recommended age to begin:
National screening program: 40 years
Opportunistic screening: No standard recommendations, usually 40 years; according to the radiologist or referring doctor.
Recommended age to stop:
National screening program: 69 years
Opportunistic screening: No standard recommendations; according to woman’s preference.
Recommended screening interval:
National screening program: 2 years
Opportunistic screening: Annual
Screening Technologies:
National screening program: 2D Digital mammography. Ultrasound is not recommended, but a warning about the low sensitivity of mammography for type C (heterogeneously dense) and D (extremely dense) breasts is given with the report.
Opportunistic screening: Digital mammography, digital breast tomosynthesis, ultrasound, automated breast ultrasound and MRI. At the discretion of the radiologist/center, ultrasound is mostly performed in women with dense breasts.
Breast density in medical mammography report: A warning about the low sensitivity of mammography in dense breasts is given in the medical mammography report in the national screening program. Electively, BI-RADS® categories are used to describe breast density in opportunistic screening.
Payment/reimbursement: National screening program covers screening digital mammography for all women over 40. In opportunistic screening, women need to have medical insurance to cover the payment; not all private medical insurance covers 100% of payment depending on the insurance plan.
High-Risk Screening:
Recommended age/modalities/interval: Women with known pathogenic BRCA1 or -2 mutations or equivalent high-risk: starting at 25, annual mammogram and MRI every year. Women who have history of receiving radiotherapy to the chest should start screening 8 years after therapy, but not sooner than age 25, with mammogram and MRI every year. Women with lifetime risk over 20% should start screening at the age risk is calculated with mammogram and MRI annually.
Sources:
Turkish Radiology Society, Breast Imaging Group: Standards for Screening:https://www.eurjbreasthealth.com/en/turkish-radiologic-society-breast-imaging-group-standarts-for-breast-cancer-screening-161922
MOH: Standards for breast cancer screening:https://hsgm.saglik.gov.tr/tr/kanser-tarama-standartlari/listesi/meme-kanseri-tarama-programı-ulusal-standartları.html
This map content provided by Prof. Dr. Erkin Aribal
Back To TopUnited Kingdom
Screening Process:
National Health Service Breast Screening Programme (NHSBSP): Mammography call and recall programme based upon Family Practitioner Register. Mobile or static unit – organised from a limited number of centres. Specialist assessment units in charge of reporting and work-up of abnormal results. All staff trained at National Training Centres. Radiologists and other groups have detailed working and performance requirements. Centralised data collection with publication of annual results. There is also opportunistic screening in the private sector.
Recommended age to begin:
National (organized) screening programme: 50 years. Current trial also inviting some women 47-49 years.
Private sector: Usually ranges from 40-45 years for women of perceived normal risk.
Recommended age to stop:
National screening programme: Women over 70 years may self-refer but will not be formally invited unless part of a separate trial inviting women aged 71-73 years.
Private sector: Screening continues until 70-80+ years according to individual policy and woman’s preference.
Recommended screening interval:
National screening programme: Every 3 years.
Private sector: Usually 1-2 years.
Screening Technologies:
National screening programme: Digital mammography
Private sector: Digital mammography. Tomosynthesis in some centres. Ultrasound and MRI occasionally performed for supplemental screening.
Breast density in medical mammography report: National screening programme: not routinely recorded. In the private sector, no specific guidelines but some centres will document breast density and explain the issue and suggest supplemental imaging – usually ultrasound if not already performed. When included, BI-RADS® categories are used to describe breast density.
Payment/reimbursement: Free of charge through the national screening programme to registered women. In the private sector, most UK medical insurance companies do not reimburse breast screening. Some women will receive corporate screening as a work benefit.
High-Risk Screening:
Recommended age/modalities/interval: Women with known pathogenic BRCA1 or -2 mutations or specific high-risk (>30% lifetime risk) categories are outlined by National Institute for Health and Care Excellence (NICE) and are recommended for annual MRI where appropriate. Eligible women can be referred to special NHSBSP Clinics.
This map content provided by Dr. Nick Perry; Dr. Anmol Malhotra
Reviewed May 2022
Back To Top