Smaller breasts tend to be dense, and large breasts are more often relatively fatty, but there is wide variation at the individual level.
E.U.
Is breast size related to breast density?
Smaller breasts are more likely to be dense, and larger breasts are more likely to be fatty, but density and size both vary from person to person.
Learn More:
If a woman has dense breasts, will she always?
Breasts tend to become less dense as women get older (see Figure below), especially after menopause, as the glandular tissue atrophies and the breast may appear more fatty-replaced. Taking hormones for menopausal symptoms can delay the regression of dense tissue. If a patient loses a lot of weight, her breasts may appear denser due to the relative loss of fat. There is also variability in the visual assessment of breast density so that the density reported in the mammogram might be “scattered” one year and “heterogeneously dense” the next year or vice versa without any true change in breast density. In both situations, there are areas within the breast where there is some dense tissue which could mask cancer detection. In recent years, the use of automated computer-based density assessment can provide reproducible and objective quantification of breast density, avoiding inter- and intraobserver variability [1].
Is breast pain or breast tenderness related to dense breast tissue?
No. Breast pain or tenderness is not related to breast density. Breast pain that comes and goes is often because of changes in hormones due to your period and is most common on the sides of your breasts (near your arms and underarms).
Benign (not cancerous) cysts, lymph nodes, and other non-cancerous growths in your breasts may cause tenderness. Skin conditions, such as shingles, and muscle soreness, can feel like breast pain.
Does breast pain mean that I have cancer?
No, breast pain alone is rarely due to cancer. If you have a painful lump or a point of pain (that you can point to with one fingertip) that lasts several weeks, you should talk with your health care provider about having additional tests.
For more information, see Q+A, “Why does breast density matter on my mammogram?”
Learn More:
If a woman does not have dense breasts, what should she do?
Annual mammography (with tomosynthesis if available) is recommended if she is over the age of 40 and in good health. If the patient is at high risk of developing breast cancer, she may be recommended to have an MRI every year in addition to mammography.
I have been told my breasts are dense. How do I find out what category they are in?
In the U.S.A., the radiologist (the doctor who looks at your mammogram) will send a report to your health care provider after your mammogram. Your breast density category (fatty, scattered density, heterogeneously dense or extremely dense) is usually in that report. Your density category may also be in the letter you receive after your mammogram. If not, you can call either the radiologist or your health care provider to find out your density. Each state has different laws about the information you must be given about your breast density. To learn what the law is in your state, click here.
In Europe, the facility that does your mammogram may either have this information or allow you to request it. Density Request forms are available for the UK – England/Wales; Scotland; Northern Ireland; Republic of Ireland here.
Learn More:
Does having dense breasts increase the chance of dying from breast cancer?
Though there is not extensive research on this topic, one study [1] indicated that because women with dense breasts are at a greater risk of developing breast cancer, their risk of dying from breast cancer is about double that of the general population. Two other studies evaluated women with breast cancer and found an increased risk of death among women with fatty breasts; the reasons for this are not well understood [2, 3]. A recent analysis from The Netherlands showed a smaller estimated mortality reduction from screening mammography of 13% in women with dense breasts compared to 41% in women with fatty breasts. Reduced benefit from mammographic screening is attributed to the masking effect of dense tissue with tumors detected later, when they were larger, in women with dense breasts [4].
Will my breasts always be dense?
Maybe not.
- Breasts tend to become less dense with age and menopause (see Figure below), but not always.
- Breasts become more dense (denser) during pregnancy and breast feeding. This is because the glands that make milk grow and the glands themselves are part of dense breast tissue. Breast density returns to what it was before pregnancy about 2-3 months after you stop breast feeding.
- If you lose a lot of weight, your breasts may appear denser on a mammogram because there is less fat, but the amount of dense tissue stays the same.
Breasts Can Become Less Dense with Age and Menopause
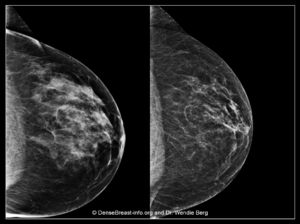
Left Image: A screening mammogram image of a premenopausal woman (age 49) shows heterogeneously dense breast tissue (Category C).
Right Image: A screening mammogram image of the same woman, now postmenopausal (age 52). Her breasts are less dense and now show scattered fibroglandular density (Category B).
Learn More:
- 5 Facts Every Woman Should Know
- Video Series: Let’s Talk About Dense Breasts
- Patient Risk Checklist (print)
- Patient Questions and Answers
If a mammography report indicates the patient has heterogeneously dense or extremely dense tissue but is otherwise categorized as “negative” or “benign” what should be considered next?
Dense breasts are “normal.” In fact, 40% of women over age 40 have dense breasts. But dense breast tissue can hide cancer on a mammogram and can reduce the effectiveness of mammography screening. So a “normal,” “negative,” or “benign” mammogram result does not reliably exclude cancer in women with dense breasts. This is why, sometimes, a woman with dense breasts may have cancer detected soon after a “normal,” “negative,” or “benign” mammogram. This is known as an “interval cancer.” To find cancer in a woman with dense breasts, additional screening should be considered. See flow chart: Who Needs More Screening? (or, in Europe, European Screening Decision Support Tool).
If I don’t have dense breasts, what should I do?
In the U.S.A., if you are age 40 or over, at average risk of developing breast cancer, and in good health, most medical societies recommend a mammogram every year (with 3D mammography/tomosynthesis, if available). If your health care provider determines that you are at high risk of getting breast cancer, a yearly MRI may be recommended to begin by age 25 to 30, with yearly mammograms beginning at age 30.
European breast cancer screening guidelines vary by country; for specific information by country, click here.
Learn More:
A patient recently had a “normal” mammogram and has extremely dense breasts. She now feels a lump. What should you recommend?
It is important for any woman not to ignore a lump just because the recent mammogram was normal, and this is especially important if the breasts are dense. While cysts, other benign masses, and areas of normal tissue can present as lumps, malignant masses, especially those lacking calcifications, are frequently masked by dense breast tissue and a “normal,” “negative,” or “benign” mammogram does not mean that there is no cancer present. Tomosynthesis can help show some cancers not found with 2D-mammography, but ultrasound is the test of choice to evaluate palpable lumps and allows targeted assessment and correlation of the area being felt with findings on ultrasound. If there is a mass suspicious for cancer, the radiologist/technologist may also include ultrasound of the tissue in the axilla (under the arm) because the first place cancer will spread is to lymph nodes in the axilla. Cancers presenting because of symptoms prior to the next annual mammogram are called “interval cancers” and interval cancers are increasingly common with increasing breast density.
What is a mammogram? Are there different types of mammograms?
Mammograms are low-dose x-rays that expose the breasts to a small amount of radiation.* Mammograms have been used to screen for breast cancer since the 1980s. There are three different types of mammograms:
- Film: 2-Dimensional, known as “analog” has been nearly eliminated in the U.S.A., but is still in use in Europe.
- Digital, 2-Dimensional: known as “Full Field Digital Mammogram” (FFDM). Nearly all facilities in the United States have digital mammography.
- Digital, 3D/tomosynthesis: also referred to as “3-Dimensional” or “tomo.” It is a newer technology that is used in over half of the facilities in the United States.
How are a 2D and 3D digital mammogram different?
To explain the difference, think of a 2D mammogram like a photograph of a book. The words on each page of the book would have their letters jumbled on top of the words from all the other pages, so it would be very difficult to read any particular word. Any given “word” could be a small mass due to cancer.
Now, to understand a 3D mammogram, imagine the cover and pages of the book are see-through. The 3D mammogram captures images at different angles, which allows thin “slice” images to be made by the computer. These images can then be viewed one at a time–similar to turning pages of a book and being able to read the words on each page.
A 2D mammogram finds about 5 cancers for every 1,000 women who have a mammogram. Another 1-2 cancers will be found per 1,000 women when 3D/tomosynthesis is used. With 3D mammograms, you are also less likely to be called back for more testing. However, in women with extremely dense breasts, studies have shown mixed results as to whether 3D mammograms find more cancers than 2D mammograms.
*The radiation exposure from a mammogram is small and is too low to cause any harm to the breasts.
To learn more about mammograms, including how they work, benefits and things to consider, click here.
Learn More:
When should screening mammography begin and stop?
Based on randomized trials (invitation to screening) mammography, there is at least a 15% decrease in deaths due to breast cancer in women screened in their 40s and a 22% reduction in deaths among women screened from ages 50 to 74 [1]. In observational studies of women actually having mammographic screening, reduction in deaths due to breast cancer is closer to 40% [2, 3]. Based on these results, the American College of Radiology (ACR) recommends annual screening beginning at age 40 for women at average risk for breast cancer [4]. The European Society of Breast Imaging (EUSOBI) recommends biennial screening mammography for average-risk women aged 50–69 years; extension up to 73 or 75 years biennially and from 40–45 to 49 years, annually [5]. Breast cancer incidence peaks earlier, in the 40s, for African American, Asian, and Hispanic women [6], than for Caucasian women when the peak is in the early 50s. As such, it is especially important for African American, Asian, and Hispanic women to start screening by age 40. The age to stop screening should be based on a woman’s overall health status. Women with a life expectancy less than 5-7 years are unlikely to realize a benefit from screening mammography.
Women at high risk for breast cancer, because of known or suspected disease-causing variants (mutations) in BRCA or other genes such as P53, should begin screening earlier; American Cancer Society recommendations, as well as those of the European Society of Mastology (EUSOMA), include annual MRI [7, 8]: BRCA-1 carriers should begin by age 25, and BRCA-2 carriers by age 30. Women with a history of radiation therapy to the chest (e.g., for Hodgkin’s disease) before age 30 should begin screening with mammography and MRI at age 25, or 8 years after treatment, whichever is later. Emerging evidence suggests that for BRCA-1 carriers who have annual MRI, the benefit of mammography is relatively small before age 40 [9]. Once a woman has had breast cancer, she should have at least annual mammography; if she also has dense breasts and/or was diagnosed with breast cancer by the age of 50, the ACR recommends she consider annual MRI in addition to mammography [10].
For other women with a family history of breast cancer, it is important to consider many factors, including the age at diagnosis of family members. Several risk models have been developed. While all models can over- or underestimate risk in a given individual, the Tyrer-Cuzick model is the most consistently accurate and, as of September 2017, includes breast density as a risk factor. For women estimated to have a lifetime risk of breast cancer of 20% or more, annual MRI screening has been recommended in addition to mammography [7, 10].
Might I have cancer even if my mammogram report is “normal”?
Yes. A “negative,” “benign,” or “normal” mammogram report does not mean cancer is not there. The denser the breast, the more likely it is that a cancer will not show on a mammogram.
| Category of Breast Density | Percent of Cancers That Will Not Show on a Mammogram |
|---|---|
| Extremely dense | 40% |
| Heterogeneously dense | 25% |
| Scattered fibroglandular | 15% |
| Fatty breasts | 10% © DenseBreast-info.org Rev. March 2022 |
Cancer can still be there even if the mammogram report is “normal.” You may want to have an additional screening test after your mammogram to help find cancer. These tests might include one of the following: Ultrasound, MRI, contrast-enhanced mammography or molecular breast imaging (MBI). If your mammogram shows dense breasts, talk with your health care provider about whether you should have an additional screening test after your mammogram.
Learn More:
Should mammography screening begin at age 40 or 50?
Women should begin screening at age 40. Though breast cancer is more common as women get older, it is still important to begin screening at 40 because:
- We screen for breast cancer to find it EARLY, when it is easier to treat and most survivable.
- Breast cancer is the number one cause of death in women aged 35 to 54 years.
- Deaths from breast cancer are reduced the most when screening starts at age 40. The most years of life are saved when screening starts at age 40.
- More than half of women in their 40s have dense breasts (heterogeneously dense or extremely dense). Dense breast tissue increases the risk for developing breast cancer and the consideration of additional screening after a mammogram.
- Women at “high risk” for breast cancer, most often because they have a disease-causing mutation (such as BRCA1 or BRCA2), should begin screening even younger – at least by age 30 and with the inclusion of an MRI.
WHAT ABOUT FALSE ALARMS (KNOWN AS “FALSE POSITIVES”)?
- About 10% of women having a screening mammogram will be called back (recalled) for extra testing or views. THIS IS NORMAL. Among women called back, 95% do not have cancer. If a needle biopsy is necessary, even that is a simple test not much different from a dental filling.
- The newer technique of 3D-mammography (also known as tomosynthesis), is better able to show cancer AND results in fewer callbacks for extra testing.
WHAT ABOUT SCREENING IN DENSE BREASTS?
- Younger women are more likely to have dense breast tissue that can hide cancer on mammography.
- In women who have breasts categorized as “dense” (heterogeneously dense or extremely dense), adding screening ultrasound after a mammogram can help find more breast cancers. However, ultrasound also finds areas/masses that are not cancer and increases the chance of needing a needle biopsy to determine if such areas/masses detected are cancerous or not.
IS IT COVERED?
- Under the Affordable Care Act, insurance carriers are required to cover the full cost of screening mammography. If the screening is performed by 3D mammography (tomosynthesis), the full cost might not be covered by some insurance companies in some states.
- Insurance coverage for additional screening tests, such as ultrasound or MRI, varies by state and by insurance company. Women should check with their insurance carriers to determine how additional tests will be covered. In women at high risk for breast cancer, most insurers will cover screening MRI (regardless of density) though a deductible/co-pay will typically apply, and pre-authorization may be needed.
- Diagnostic mammography is performed to evaluate abnormalities found on screening or when a woman has signs or symptoms of breast cancer. A deductible/co-pay will usually apply for diagnostic mammography.
If mammograms miss some cancers in dense breasts, should I still have a mammogram?
Yes. Though both 2D and 3D mammograms can miss cancers in dense breasts, mammograms are still helpful. Some cancers will only be seen on a mammogram (and won’t be seen on Ultrasound or possibly even on MRI).
For example, even in dense breasts, mammograms will show calcifications (white specks like salt crystals, see Figure below), which are seen better on mammograms than on Ultrasound. About half of all breast cancers have calcifications. However, most calcifications seen on a mammogram are not due to cancer.
Many studies have shown that finding early stage cancers on a mammogram reduces deaths from breast cancer.
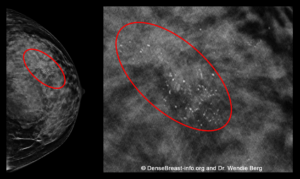 Mammograms Show About Half of Early Breast Cancers Even in Dense Breasts
Mammograms Show About Half of Early Breast Cancers Even in Dense Breasts
This mammogram of a woman with dense breasts shows a group of calcifications (white specks that are like salt crystals within the red ovals). This patient was diagnosed with invasive breast cancer (“invasive” means it has spread to surrounding breast tissue).
Learn More: