Usually the answer is yes, though age and other medical conditions will change a patient’s personal risk and benefit considerations and therefore screening recommendations may change from one year to the next. Technology is changing and guidelines also evolve which influence recommendations.
E.U.
If I am a breast cancer survivor, does having dense breasts increase the chance of getting cancer in my opposite breast?
Yes. If you have dense breasts and have had breast cancer, there is a greater chance of developing cancer in the opposite breast (known as contralateral breast cancer). The good news is that this risk can be reduced with medications.
Learn More:
Is MBI recommended for screening dense breasts?
Molecular Breast Imaging (MBI) is a specialized nuclear medicine breast imaging technique that requires intravenous injection of a radiopharmaceutical, typically 99mTc-sestamibi. Sestamibi has been in common use as a tracer for nuclear cardiology studies for over 30 years and has an extremely low risk of adverse reactions and no contraindications. Low-dose molecular breast imaging has been used with excellent results by Mayo Clinic and a few other centers for screening women with dense breasts, showing another 7 to 8 cancers after a normal mammogram for every thousand women screened [1-3].
MBI can also be useful as a diagnostic tool in women who have dense breasts and symptoms such as a lump or vague abnormality on mammography that in rare cases cannot be sorted out with additional views or ultrasound. MBI can also be helpful for some women who need but cannot have an MRI [4]. As of the most recent review in 2017, the American College of Radiology Practice Parameter for Molecular Breast Imaging [5] suggests MBI is a potential option for supplemental screening in high-risk women and those with dense breasts who cannot undergo MRI, but it is usually not indicated, as the technique involves ionizing radiation to the whole body with attendant risk of potentially inducing cancer [6]. MBI is never used in women who are pregnant.
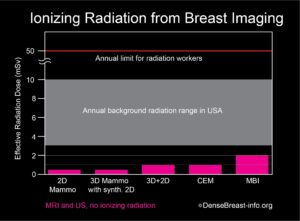
The radiation exposure from low-dose MBI, performed with a delivered dose of 6 to 8 mCi 99mTc-sestamibi, is higher than that from a mammogram. Further, mammography delivers radiation to the breast only, while MBI delivers radiation to the whole body. In order to compare radiation doses from these different types of exams, a standard calculation called “effective radiation dose” is used, which takes into account which body parts are exposed to radiation by a given test and how sensitive every exposed organ is to radiation. Effective dose has units of milli-Sieverts (mSv). The effective dose of mammography is about 0.5 mSv and the effective dose from a low-dose MBI is about 1.8 to 2.4 mSv. For comparison, the radiation dose received from normal daily life is between 3 and 10 mSv per year, depending on where you live [7, 8]. Below effective doses of 100 mSv, no health risks from radiation have been proven according to national and international radiation physics experts [9-11].
Chart 1. This graph shows the whole body effective radiation doses from common breast screening exams: 2D mammography; 3D (tomosynthesis) mammography with synthetic 2D; 2D combined with 3D mammography; contrast-enhanced mammography (CEM); and molecular breast imaging (MBI). MBI, with the highest dose, at 2 mSv, is below the range of annual background radiation exposure in the USA. The annual limit for radiation workers is 50 mSv. At doses below 100 mSv, no risks have been proven, and benefits to patients outweigh any possible risks. Any risk from radiation is greater in younger individuals, especially those under the age of 30, and radiation exposure should always be minimized (except when undergoing cancer treatment).
Are lumpy or fibrocystic breasts the same thing as dense breasts?
No. Having “lumpy” or fibrocystic breasts is different than having dense breasts, but some women have both.
Normal breast tissue can feel lumpy whether it is fatty or dense. Cysts are common and noncancerous and sometimes are large enough to be noticed as a lump. Having dense breasts has nothing to do with the way your breasts look or feel. The doctor who reviews your mammogram determines whether you have dense breasts after looking closely at images from your mammogram.
Learn More:
Should thermography be used to screen dense breasts?
No. According to the FDA, “There is no valid scientific data to demonstrate that thermography devices, when used on their own or with another diagnostic test, are an effective screening tool for any medical condition including the early detection of breast cancer or other diseases and health conditions [1].”
Thermography is a non-invasive technique that uses infrared technology to detect both heat and blood flow patterns very near the skin’s surface. Although some large cancers can be seen, these are usually palpable and so thermography adds little. Thermography has a high “false negative” rate (when a test result indicates “no cancer” – though cancer is actually present), especially for small breast cancers, so it does not play a role in screening asymptomatic women. Thermography also has a high rate of “indeterminate” findings, which on additional diagnostic evaluation (mammography, ultrasound, MRI, follow-up observation, etc.) indicate no cancer is found. These often prompt a recommendation for short interval follow-up, which creates anxiety and additional cost to the woman.
Do men have dense breasts?
No. Normal male breasts do not contain dense tissue.
Sometimes men’s breasts do grow and look more like female breasts (known as gynecomastia). This can happen as men age or can be caused by some medicines.
It is important to remember that men can also get breast cancer. A mammogram can be done in men to check a lump.
Learn More:
Can the decision on supplemental screening this year be based on patient’s breast density last year?
The answer is essentially “yes”. At the population level, there is a tendency for slight decrease in breast density each year, and this tends to be more abrupt in the few years around menopause. One study [1] showed that only 7% of women who were considered not dense one year were classified as “dense” the following year; similarly 6% of women considered “dense” one year were classified as not dense the following year. For 87% of women, there was no change from one year to the next. Any difference that might affect the decision for supplemental screening would be between women considered to have heterogeneously dense or scattered fibroglandular density one year or the other, and radiologists may differ in this assessment even when there is no true change in the breasts. In a patient with breast density near the threshold, there are likely to be areas in the breast where cancer could be masked: it is not unreasonable to have had supplemental screening even if one’s breasts turn out to be slightly less dense this year.
Is breast density inherited?
If your mother or sister has dense breast tissue, it’s more likely you will too.
Learn More:
What is Dedicated Breast PET (Positron Emission Mammography, PEM)?
What is it?
Breast PET uses an injection of a short-lived radioactive sugar (18FDG) into the body to detect metabolically active lesions such as cancer. PET, or more often PET-CT, is commonly used to stage the whole body in patients with larger breast cancers or suspected recurrence. Newer technologies can provide detailed PET images of the breasts to assess local extent of breast cancer.
How it works
The radioactive sugar accumulates in cancer cells in the breast and emits high-energy positron radiation that is detected and analyzed. For one such system, the patient is seated and the breast is gently stabilized; positioning is otherwise like mammography (Fig. PET-1).


Benefits
Breast PET is generally considered a diagnostic test used to determine the extent of cancer within the breasts, and can be used as an alternative to breast MRI for that purpose [1, 2]. In women with newly diagnosed breast cancer being treated with chemotherapy prior to surgery, breast PET can also help monitor response to treatment. In addition, breast PET may help distinguish recurrence of cancer from scar in women who have been previously treated for breast cancer. Uncommonly, it can be used for problem solving (Fig. PET-3). It is a relatively new modality and not widely available.
Considerations
Breast PET exposes the patient to a moderately high whole body radiation dose and is not used for screening [3]. The very back part of the breast near the chest wall and the axillary lymph nodes are better evaluated with MRI.

Do Black women have denser breasts? Do Asian women have denser breasts? Do Hispanic women have denser breasts?
Many studies have found that Asian women more often have dense breasts than women of other races. Studies differ on whether Black or Hispanic women have denser breasts than non-Hispanic white women.
What matters most is your individual breast density. If you have dense breasts, you are more likely to get breast cancer and it is more likely to be missed on the mammogram.
Learn More:
Can breast density be changed with diet? Is fat in the diet related to breast density?
Dietary fat intake has little to do with breast density; however, it does relate to increased body mass index (BMI). BMI is a measure of body fat based on height and weight, and there is more fatty breast tissue in women with higher BMI. Higher BMI reduces the percent of density but might not reduce the total amount of dense tissue. BMI and breast density are both separate risk factors for breast cancer. Before menopause, low BMI [1, 2] increases the risk of breast cancer. After menopause, weight gain and increasing BMI increase the risk of breast cancer.
What if I have dense breasts and a disease-causing BRCA gene variant (mutation)?
Disease-causing BRCA gene variants and dense breasts both increase the chances that a woman will get breast cancer. However, BRCA1 or BRCA2 variants put women at a much higher risk for getting breast cancer than the risk from having dense breasts.
Because BRCA gene carriers are more likely to get breast cancer at a younger age, they usually get a breast Magnetic Resonance Imaging (MRI) as part of their breast screening. In these women, breast screening should also start earlier, with MRI beginning at age 25 and mammography starting at age 30 or later.
MRI screening for women with BRCA variants is suggested whether or not they have dense breasts.
Learn More:
Can exercise affect a woman’s breast density category?
It can. While exercise can decrease the amount of fat in the breast, the glandular or dense breast tissue is not affected by exercise. So, if a woman loses a lot of weight due to exercise, her breasts can appear more dense due to loss of fat (the amount of fat decreases while the amount of dense tissue remains the same) [1].
While exercise does not decrease the actual amount of dense tissue in the breasts, it does decrease the overall risk of developing breast cancer [2].
Does taking hormone replacement therapy (HRT) or estrogen therapy alone affect breast density or breast cancer risk?
- Increases in both breast density [1, 2] and breast cancer risk [3, 4] have been shown in patients taking oral or transdermal combined estrogen and progesterone hormone supplements (i.e. hormone replacement therapy, HRT).
- In women who have had breast cancer, oral or transdermal HRT have been shown to increase risk of breast cancer recurrence [5].
- Data are conflicting as to whether taking oral or transdermal estrogen alone in women who have had a hysterectomy increases breast density [5-9] or breast cancer risk [3, 4].
- There are minimal data on the effect of vaginal estrogen on breast density.
- In women who have not had breast cancer, vaginal estrogen has not been shown to increase breast cancer risk.
- In women who have had breast cancer, vaginal estrogen has not been shown to increase breast cancer recurrence, except in one study that reported an increased risk in breast cancer survivors who took aromatase inhibitors [6]. Vaginal estrogen has not been shown to increase death from breast cancer in breast cancer survivors [6, 13].
A large meta-analysis of prospective observational studies found that ever users of HRT had a 30% greater risk of developing breast cancer than never users [relative risk (RR) 1.29 (95% CI 1.27, 1.30)][3]. Risk increased with duration of use for both current and past users, with higher risk at any given duration of use for current users [current users, RR 1.20 (95% CI 1.01-1.43) for <1 year of use to 2.51 (95% CI 2.35-2.68) for ≥ 15 years of use; past users, RR 1.02 (95% CI 0.95-1.10) for <1 year of use to 1.30 (95% CI 1.25-1.37) for ≥ 15 years of use]. Similarly, the Women’s Health Initiative randomized trial found nearly 30% greater risk after a median 20 years of follow-up among women randomized to estrogen and medroxyprogesterone acetate (hazard ratio 1.28; 95% CI 1.13-1.45) [4].
Data are conflicting as to whether taking oral or transdermal estrogen alone in women who have had a hysterectomy increases breast density [7-11] or breast cancer risk [3, 4]. There are minimal data on the effect of vaginal estrogen on breast density. Vaginal estrogen has not been shown to increase breast cancer risk [3, 12] in women who have not had breast cancer.
In women who have had breast cancer, oral or transdermal HRT have been shown to increase risk of breast cancer recurrence [5]. Vaginal estrogen has not been shown to increase risk of breast cancer recurrence, except in one study that reported an increased risk in breast cancer survivors who used vaginal estrogen and took aromatase inhibitors [6]. Vaginal estrogen has not been shown to increase death from breast cancer in women who have had breast cancer [6, 13].
Is there anything a patient can do to decrease her breast density? What about taking tamoxifen?
Tamoxifen blocks the estrogen receptor in breast cells and in breast cancer cells which express the estrogen receptor. Tamoxifen may be recommended to reduce the risk of developing breast cancer in women who have had prior atypical biopsies. Tamoxifen is also prescribed for women who have had breast cancer that expresses estrogen receptors to decrease recurrence. One study [1] found that when breast density is carefully measured by computer software, women whose breasts became at least 10% less dense while taking tamoxifen had a 63% reduction in risk of developing breast cancer – whereas those whose breast density did not change did not see a decrease in their risk. Several similar studies [2, 3] in women who have had breast cancer showed that only women whose breast density decreased on tamoxifen had decreased risk of recurrence. Tamoxifen also carries about a 3% risk of blood clots (which could result in pulmonary embolism or stroke) and a smaller risk of endometrial cancer (if the woman still has her uterus).
If a woman is on hormone therapy for menopausal symptoms, her breast density may decrease if she stops taking hormone supplements.
Will taking Arimidex or other aromatase inhibitors affect breast density?
Aromatase inhibitors block the body’s own production of estrogen and are prescribed for postmenopausal women who have had breast cancer where the tumor cells express receptors for estrogen. One study [1, 2] looked at women who have had breast cancer. When breast density is carefully measured by computer software, women who experienced a decrease in breast density while taking tamoxifen or aromatase inhibitors had a lower risk of recurrence than women who did not experience a decrease in breast density.