Complete List of Questions and Answers
What Is Breast Density and Why Does It Matter?
1. What are dense breasts?
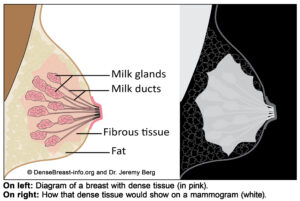
“Dense breasts” are words that describe the mix of fat, milk glands/milk ducts and fibrous tissue in a breast. The more glands and fibrous tissue a woman has (also called “fibroglandular” tissue), the “denser” her breast tissue.
Each woman has a unique mix of fatty and dense tissue in her breasts. Some women have very little dense tissue compared to fatty. Other women have more dense tissue compared to fatty. Most women’s breasts are somewhere in-between.
Are Dense Breasts Normal?
Dense breasts are normal and common. Dense breasts are not caused by illness or disease. But there are some reasons for concern. That is because dense breasts can make it harder for radiologists to find cancer on a mammogram. Also, dense breasts increase a woman’s risk for breast cancer.
Here is more to know:
- Dense tissue appears as light gray or white on a mammogram (see image on the right). In dense breasts, any lump (whether due to cancer, or not) can also look light gray or white. That makes it harder for radiologists to find cancers on a mammogram for women who have dense breasts. It is like trying to find a snowball in a blizzard.
- Dense breasts are a risk factor for breast cancer. A woman’s risk for breast cancer increases with the level of density in her breast. Please see Q+A #6 “Do dense breasts affect my risk of getting breast cancer?”.
Learn More:
2. What causes dense breast tissue?
Dense breasts are normal and are not caused by illness. All breasts are made of fat, and milk ducts/milk glands held together by fibrous tissue. The glands and fibrous tissue (or “fibroglandular” tissue) are referred to as “dense tissue”.
Each woman’s breasts are different and contain their own mix of fatty and dense tissue. Some women have breasts made of mostly fatty tissue. Some women have breasts with a lot of dense tissue. The more glands and fibrous tissue that a woman has, the “denser” her breast tissue is.
How can I tell if I have dense breasts?
The radiologist (the doctor who looks at your mammogram) can tell how dense your breasts are by how they look on your mammogram. You cannot tell if you have dense breasts by the way your breasts look or feel.
Learn More:
3. Women often ask how to diagnose dense breast tissue. “How is breast density on a mammogram determined?”
Radiologists are the doctors who determine whether a woman has dense breasts. They do so after looking closely at images from mammograms. Radiologists may also use computer software to measure breast density. Breast density cannot be determined by how a breast looks or feels.
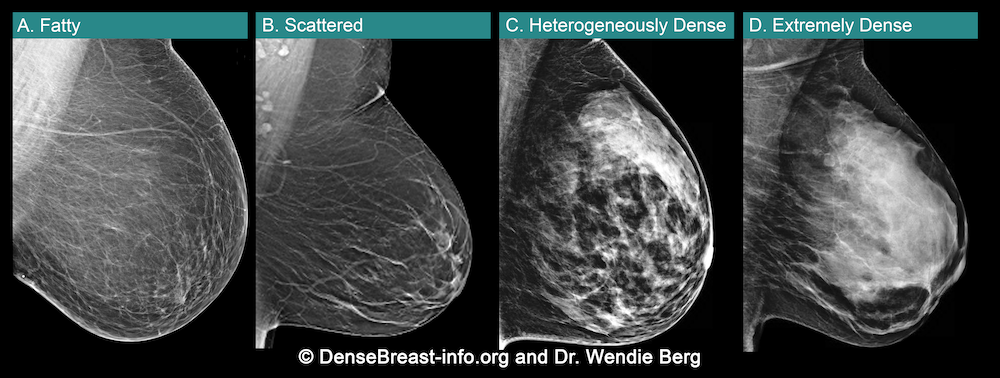
There are 4 categories of breast density. Here is more to know about each category:
Category A. Fatty, or almost entirely fatty breasts. This means that most of the breast is made of fat tissue. On a mammogram, a fatty breast appears as mostly dark grey or black. While most of the breast is fatty tissue, there may be a small amount of dense (fibroglandular) tissue that looks light grey or white. About 10% of all women have fatty breasts. Breasts in Category A are not considered dense.
Category B. Scattered areas of fibroglandular density. The breast has a mix of fatty tissue which appears dark grey or black, and scattered dense (fibroglandular) tissue which looks light grey or white. It can be hard for radiologists to find cancer, which often also look light grey or white, in areas that are dense. About 40% of all women have this type of breast. Breasts in Category B are not considered dense.
Category C. Heterogeneously dense breasts. Large portions of the breast are made of dense (fibroglandular) tissue. On a mammogram, the breast appears mostly light grey or white. It is harder for radiologists to find cancer, which often also looks light grey or white. About 40% of all women have heterogeneously dense breasts. Breasts in Category C are considered dense.
Category D. Extremely dense breasts. Most of the breast is made of dense (fibroglandular) tissue. On a mammogram, the breast looks almost all white. This makes it very hard for radiologists to find cancer, which often also looks light grey or white. About 10% of all women have extremely dense breasts. Breasts in Category D are considered dense.
Learn More:
4. Do you know your breast density? Are you dense?
In Europe, the facility that does your mammogram may either have this information or allow you to request it. Density Request forms are available for the UK here.
In the U.S.A. the FDA now requires that after a mammogram, all patients be told whether their breasts are “dense” or “not dense.” Click here to see what you must be told about breast density after your mammogram. If you would like to also learn which specific density category your breasts are (heterogeneously dense or extremely dense), you can: (1) ask the place where you had your mammogram, or (2) ask your referring health care provider (that information is included in the report sent to them).
Learn More:
5. Why does breast density matter on my mammogram?
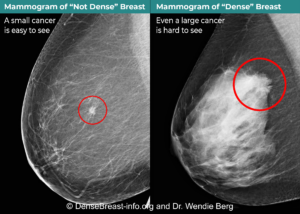
Cancers can be hidden or “masked” by dense tissue. On a mammogram, cancer is white. Normal dense tissue also appears white. If a cancer grows in an area of normal dense tissue, it can be hard or even impossible to see cancer on a mammogram.
It is like trying to see a snowball in a blizzard.
- If a cancer (white) develops in an area of fat (black or dark gray/grey), it is usually easy to see cancer even when it is small. The more fatty a breast is, the easier it is to see cancer on a mammogram.
- Dense breast tissue can hide cancers. The denser a breast is, the harder it is to see cancer on a mammogram.
Cancer on a Mammogram in a Fatty Breast vs. a Dense Breast
Learn More:
6. Do dense breasts affect my risk of getting breast cancer?
Yes. Dense breasts not only can hide cancer on a mammogram, but they also increase the risk of getting breast cancer. Cancers grow more often in dense tissue than in fatty tissue. The denser the breasts are, the higher the breast cancer risk. Women with the densest breasts (“extremely dense”) are 4 times more likely to get breast cancer than women with the least dense breasts (“fatty” breasts). Most women’s breasts have density in between these two categories (“scattered fibroglandular density” or “heterogeneously dense” breasts).
What are risk factors for breast cancer?
Most breast cancer occurs in women with no known risk factors other than being a woman and getting older. There are many risk factors that increase the chance of getting breast cancer. For example:
- Having dense breasts
- Having a family history of breast or ovarian cancer (particularly in your mother or sisters)
- Having an atypical breast biopsy (where breast cells from a small sample of your breast tissue were not normal, but not yet cancer)
Learn More:
References
1. American Cancer Society. Breast Cancer Facts & Figures 2019-2020. Atlanta: American Cancer Society, Inc. 2019. Retrieved from https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/breast-cancer-facts-and-figures-2019-2020.pdf. Accessed April 20, 2020.
2. McCormack VA, dos Santos Silva I. Breast density and parenchymal patterns as markers of breast cancer risk: A meta-analysis. Cancer Epidemiol Biomarkers Prev 2006; 15:1159-1169
7. Should I worry about dense breast tissue? Are dense breasts abnormal?
Dense breasts are normal and common. Though normal, dense breasts do increase the risk of developing breast cancer and of having a cancer missed on a mammogram.
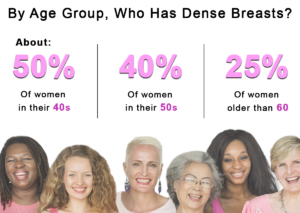
Many women have dense breasts. Density tends to decrease as a woman gets older.
Talk to your doctor about whether you should have additional tests after your mammogram.
Learn More:
What Should I Know About Dense Breasts?
8. Are dense breasts common? Is it unusual to have dense breasts?
 Dense breasts are normal and common and can change over time. Younger women tend to
Dense breasts are normal and common and can change over time. Younger women tend to
have denser breasts. Breasts tend to become less dense around menopause when estrogen
(a hormone) levels drop.
Why do dense breasts matter?
Dense breasts matter because dense tissue can hide cancer on a mammogram. Dense breasts also increase the risk of developing breast cancer. If you have dense breasts, you may need another test in addition to your mammogram to find cancer (if present).
Learn More:
9. Is breast size related to breast density?
Smaller breasts are more likely to be dense, and larger breasts are more likely to be fatty, but density and size both vary from person to person.
Learn More:
10. Is breast pain or breast tenderness related to dense breast tissue?
No. Breast pain or tenderness is not related to breast density. Breast pain that comes and goes is often because of changes in hormones due to your period and is most common on the sides of your breasts (near your arms and underarms).
Benign (not cancerous) cysts, lymph nodes, and other non-cancerous growths in your breasts may cause tenderness. Skin conditions, such as shingles, and muscle soreness, can feel like breast pain.
Does breast pain mean that I have cancer?
No, breast pain alone is rarely due to cancer. If you have a painful lump or a point of pain (that you can point to with one fingertip) that lasts several weeks, you should talk with your doctor about having additional tests.
For more information, please see Q+A #15, “Why does breast density matter on my mammogram?”.
Learn More:
11. I have been told my breasts are dense. How do I find out what category they are in?
In Europe, the facility that does your mammogram may either have this information or allow you to request it. Density Request forms are available for the UK – England/Wales; Scotland; Northern Ireland; Republic of Ireland here.
In the U.S.A., the radiologist (the doctor who looks at your mammogram) will send a report to your health care provider after your mammogram. Your breast density category (fatty, scattered density, heterogeneously dense or extremely dense) is in that report. Your density category may also be in the letter you receive after your mammogram.
Learn More:
12. Will my breasts always be dense?
Maybe not.
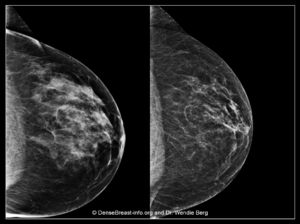
- Breasts tend to become less dense with age and menopause (see Figure below), but not always.
- Breasts become more dense (denser) during pregnancy and breast feeding. This is because the glands that make milk grow and the glands themselves are part of dense breast tissue. Breast density returns to what it was before pregnancy about 2-3 months after you stop breast feeding.
- If you lose a lot of weight, your breasts may appear denser on a mammogram because there is less fat, but the amount of dense tissue stays the same.
Breasts Can Become Less Dense with Age and Menopause
Left Image: A screening mammogram image of a premenopausal woman (age 49) shows heterogeneously dense breast tissue (Category C).
Right Image: A screening mammogram image of the same woman, now postmenopausal (age 52). Her breasts are less dense and now show scattered fibroglandular density (Category B).
Learn More:
13. If I don’t have dense breasts, what should I do?
European breast cancer screening guidelines vary by country; for specific information by country, click here.
In the U.S.A., if you are age 40 or over, at average risk of developing breast cancer, and in good health, most medical societies recommend a mammogram every year (with 3D mammography/tomosynthesis, if available). If your health care provider determines that you are at high risk of getting breast cancer, a yearly MRI may be recommended to begin by age 25 to 30, with yearly mammograms beginning at age 30.
Learn More:
What Do I Need to Know About Mammograms and Dense Breasts?
14. What is a mammogram? Are there different types of mammograms?
Mammograms are low-dose x-rays that expose the breasts to a small amount of radiation.* Mammograms have been used to screen for breast cancer since the 1980s. There are three different types of mammograms:
- Film: 2-Dimensional, known as “analog” has been nearly eliminated in the U.S.A., but is still in use in Europe.
- Digital, 2-Dimensional: known as “Full Field Digital Mammogram” (FFDM). Nearly all facilities in the United States have digital mammography.
- Digital, 3D/tomosynthesis: also referred to as “3-Dimensional” or “tomo.” It is a newer technology that is used in over half of the facilities in the United States.
How are a 2D and 3D digital mammogram different?
To explain the difference, think of a 2D mammogram like a photograph of a book. The words on each page of the book would have their letters jumbled on top of the words from all the other pages, so it would be very difficult to read any particular word. Any given “word” could be a small mass due to cancer.
Now, to understand a 3D mammogram, imagine the cover and pages of the book are see-through. The 3D mammogram captures images at different angles, which allows thin “slice” images to be made by the computer. These images can then be viewed one at a time–similar to turning pages of a book and being able to read the words on each page.
A 2D mammogram finds about 5 cancers for every 1,000 women who have a mammogram. Another 1-2 cancers will be found per 1,000 women when 3D/tomosynthesis is used. With 3D mammograms, you are also less likely to be called back for more testing. However, in women with extremely dense breasts, studies have shown mixed results as to whether 3D mammograms find more cancers than 2D mammograms.
*The radiation exposure from a mammogram is small and is too low to cause any harm to the breasts.
To learn more about mammograms, including how they work, benefits and things to consider, click here.
Learn More:
15. Might I have cancer even if my mammogram report is “normal”?
Yes. A “negative,” “benign,” or “normal” mammogram report does not mean cancer is not there. The denser the breast, the more likely it is that a cancer will not show on a mammogram.
| Category of Breast Density | Percent of Cancers That Will Not Show on a Mammogram |
|---|---|
| Extremely dense | 40% |
| Heterogeneously dense | 25% |
| Scattered fibroglandular | 15% |
| Fatty breasts | 10% © DenseBreast-info.org Rev. March 2022 |
Cancer can still be there even if the mammogram report is “normal.” You may want to have an additional screening test after your mammogram to help find cancer. These tests might include one of the following: Ultrasound, MRI, contrast-enhanced mammography or molecular breast imaging (MBI). If your mammogram shows dense breasts, talk with your doctor about whether you should have an additional screening test after your mammogram.
Learn More:
References
1. Kerlikowske K, Zhu W, Tosteson AN, et al. Identifying women with dense breasts at high risk for interval cancer: a cohort study. Ann Intern Med 2015; 162:673-681
2. Wanders JO, Holland K, Veldhuis WB, et al. Volumetric breast density affects performance of digital screening mammography. Breast Cancer Res Treat 2017; 162:95-103
16. If mammograms miss some cancers in dense breasts, should I still have a mammogram?
Yes. Though both 2D and 3D mammograms can miss cancers in dense breasts, mammograms are still helpful. Some cancers will only be seen on a mammogram (and won’t be seen on Ultrasound or possibly even on MRI).
For example, even in dense breasts, mammograms will show calcifications (white specks like salt crystals, see Figure below), which are seen better on mammograms than on Ultrasound. About half of all breast cancers have calcifications. However, most calcifications seen on a mammogram are not due to cancer.
Many studies have shown that finding early stage cancers on a mammogram reduces deaths from breast cancer.
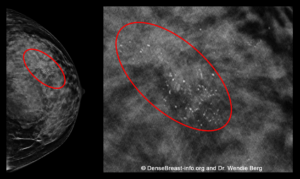 Mammograms Show About Half of Early Breast Cancers Even in Dense Breasts
Mammograms Show About Half of Early Breast Cancers Even in Dense Breasts
This mammogram of a woman with dense breasts shows a group of calcifications (white specks that are like salt crystals within the red ovals). This patient was diagnosed with invasive breast cancer (“invasive” means it has spread to surrounding breast tissue).
Learn More:
17. I have dense breasts and cancer might be missed on my mammogram, what other screening tests can I do?
18. My recent mammogram was “normal,” but I feel a lump. What should I do?
You should not ignore a lump or any change in your breasts just because your recent mammogram was “normal.” This is especially important if your breasts are dense. While lumps are often cysts or areas of normal tissue, a lump may be cancer that is hidden within dense breast tissue on a mammogram. If you have a lump, you should talk to your doctor and have a “diagnostic” breast imaging appointment where often an Ultrasound will be performed.
A “normal,” “negative,” or “benign” screening mammogram report does not necessarily mean there is no cancer.
Learn More:
19. Can I just have screening ultrasound and skip mammography?
No. Ultrasound is not a replacement or substitute for mammography. Some breast cancers are only detected by 2D or 3D/tomosynthesis mammography, even in dense breasts.
Learn More:
20. I am a breast cancer survivor and have dense breasts. Is a mammogram enough screening for me?
Maybe not. Women who have had breast cancer are more likely to get a second breast cancer. Some of these cancers are hard to see on a mammogram. In women who have had breast cancer, MRI can help find cancers not seen on a mammogram.
You should talk to your doctor about having an annual MRI in addition to a 2D/3D mammogram if:
- You were diagnosed with breast cancer by age 50
- If you have a history of breast cancer and dense breasts
- You are younger than 70-75
If MRI cannot be performed, Ultrasound can be used, but it does not find as many cancers as MRI. If you have a screening MRI, a screening Ultrasound is not needed.
A newer breast imaging tool is contrast-enhanced mammography. This may be an option instead of an MRI. It does show more cancers than Ultrasound, but it is not yet widely available.
If you have had both breasts removed (double mastectomy) and are otherwise in good health, mammograms or other breast imaging tests are not recommended unless there is a lump or other change in the area of surgery or your underarm.
Learn More:
References
1. Monticciolo DL, Newell MS, Moy L, Niell B, Monsees B, Sickles EA. Breast cancer screening in women at higher-than-average risk: Recommendations from the ACR. J Am Coll Radiol 2018; 15:408-414
21. At what age should I start getting mammogram screenings?
If you live in Europe, recommendations vary by country; click here to learn more. Most medical societies in the U.S.A. recommend women begin getting mammograms by age 40.*
The goal of mammogram screenings is to find breast cancer EARLY, when it is easier to treat and most survivable.
Though breast cancer is more common as women get older, it is important to begin mammogram screenings by age 40 because:
- Breast cancer is the number one cause of death in women aged 35 to 54 years.
- Beginning by age 40 lowers the chance of dying from breast cancer.
- Beginning by age 40 is especially important for Asian, Hispanic or Black women as they are more often diagnosed with breast cancer at a younger age.
- More than half of women in their 40s have dense breasts (heterogeneously dense or extremely dense). Dense breasts increase the risk of developing breast cancer and can hide cancer on a mammogram. Women with dense breasts should talk to their doctor about additional screening after their mammogram.
* Women at “high risk” for breast cancer (for example, those who have a disease-causing genetic mutation such as BRCA1 or BRCA2), should begin getting mammograms even younger – at least by age 30 — and also get an MRI every year.
Learn More:
22. What is a recall and what is a false positive from a mammogram?
About 1 in every 10 women who have a screening mammogram will be called back or “recalled” for extra views or screening tests to look at an area of the breast more closely. THIS IS EXPECTED.
- It is much more common for women to be recalled after their very first mammogram. This is because there is no prior mammogram for comparison to know what is normal for your breasts.
- Among women called back, most (95%) do not have cancer. These are considered false positives or “false alarms.”
Usually, extra mammogram pictures or an ultrasound can clear up a question raised on a mammogram.
About 1 in 5 women called back for additional testing will need a needle biopsy. This is a minor in-office procedure to take a very small sample of breast tissue for testing.
Learn More:
I Have Been Told I Have Dense Breasts, What Should I Do?
23. Does insurance cover my mammogram and any additional tests?
In Europe, national breast screening programs for women of average risk are offered in nearly all countries. Variations do exist on the ages and risk factors of women invited to participate in routine screening, how often screening is recommended, and supplemental screening tools used. For specific information by European country, click here.
In the U.S.A, under the Affordable Care Act (Obamacare), insurance carriers are required to cover the full cost of a screening mammogram. A screening mammogram is for women with no symptoms. If the screening is performed by 3D/tomosynthesis mammography, the full cost might not be covered by some insurance companies. It depends on the state in which you live (click here to learn more) and what insurance you have.
- Insurance coverage for additional screening tests after your mammogram, such as Ultrasound or MRI, varies by state and by insurance company. You should check with your insurance carrier(s) to learn if and how additional tests will be covered.
- For women at high risk for breast cancer, most insurers will cover a screening MRI (regardless of density), though a deductible/co-pay may apply, and pre-authorization may be needed.
- A diagnostic mammogram is for women with a sign or symptom of breast cancer, such as a lump or nipple discharge. A diagnostic mammogram is also used if additional mammography views are needed to clear up a question raised on a screening mammogram. A deductible/co-pay will usually apply for a diagnostic mammogram. But again, it depends on where you live and your insurance plan.
Learn More:
24. If I have a 3D/tomosynthesis mammogram, do I also need a screening Ultrasound or MRI?
Yes, you may still need more screening if you have dense breasts and/or are at high risk for breast cancer. Ultrasound or especially MRI might find cancer even if your 3D mammogram is “normal.”
It is still important to have your mammogram first, as mammograms sometimes show some cancers that Ultrasound or MRI may not. The combination of tests finds the most cancers.
Learn More:
References
1. Tagliafico AS, Mariscotti G, Valdora F, et al. A prospective comparative trial of adjunct screening with tomosynthesis or ultrasound in women with mammography-negative dense breasts (ASTOUND-2). Eur J Cancer 2018; 104:39-46
2. Destounis S, Arieno A, Morgan R. Comparison of cancers detected by screening ultrasound and digital breast tomosynthesis. Abstract 3162. In: American Roentgen Ray Society (ARRS). New Orleans, LA, 2017
3. Tagliafico AS, Calabrese M, Mariscotti G, et al. Adjunct screening with tomosynthesis or ultrasound in mammography-negative dense breasts (ASTOUND): Interim report of a prospective comparative trial. J Clin Oncol 2016
4. Dibble EH, Singer TM, Jimoh N, Baird GL, Lourenco AP. Dense breast ultrasound screening after digital mammography versus after digital breast tomosynthesis. AJR Am J Roentgenol 2019; 213:1397-1402
5. Comstock CE, Gatsonis C, Newstead GM, et al. Comparison of abbreviated breast MRI vs digital breast tomosynthesis for breast cancer detection among women with dense breasts undergoing screening. Jama 2020; 323:746-756
25. If I have dense breasts, should my routine annual mammogram be scheduled as a “screening” or a “diagnostic” mammogram?
A “screening” mammogram. Screening mammograms are for women with no signs or symptoms of breast cancer, whether or not they have dense breasts, family history of breast cancer, or other risk factors. In the U.S.A., screening mammograms are fully covered by insurance under the Affordable Care Act for women over the age of 40. They may also be covered for younger women if recommended by their physician and depending on their health insurance policy.
“Diagnostic” mammograms are used when there are signs and symptoms of breast cancer such as a lump, bloody or clear nipple discharge (not milk from breast feeding) or pulling in of the skin or nipple (called retraction). Diagnostic mammograms are also used to look at areas seen on earlier mammograms (like a screening mammogram) that need more pictures or closer follow-up. “Diagnostic” mammograms start with the same images as screening but are reviewed by the radiologist at the time of the mammogram and while the patient is there. A diagnostic mammogram is usually covered by insurance but out-of-pocket costs like a deductible and copay may be required.
Learn More:
26. If I am recommended to have more tests after my mammogram (like Ultrasound or MRI), will I need to have that every year?
Maybe. You should discuss this with your doctor or Breast Imaging Radiologist. As you get older, your personal risk factors and how you might benefit from more screening after your mammogram may change. It is important to talk about your risk factors every year or two with your doctor to determine what screening plan is best for you.
Learn More:
27. Is MBI recommended for screening women with dense breasts?
Molecular Breast Imaging (MBI) is a breast imaging test that use a small amount of radioactive material. This test can find cancers hidden within dense breast tissue on a mammogram, but is not usually recommended for breast cancer screening because the radiation from MBI is to the whole body. This is not like a mammogram, where only the breasts receive radiation (in a very small amount), and not like an Ultrasound or MRI, where there is no ionizing radiation at all.
MBI is not used in women who are pregnant.
For more information about MBI, click here.
Learn More:
References
1. Rhodes DJ, Hruska CB, Conners AL, et al. JOURNAL CLUB: Molecular breast imaging at reduced radiation dose for supplemental screening in mammographically dense breasts. AJR Am J Roentgenol 2015; 204:241-251
28. Is thermography helpful in finding cancers in dense breasts?
No. Thermography is not an accurate test and is not recommended for screening. For additional information on thermography from the United States Food and Drug Administration, click here.
Learn More:
What Are Factors That May Affect Breast Density?
29. Can I lower my breast density?
There are no guidelines or suggestions on how women can lower breast density, but some medications have been shown to help:
- For women who have had estrogen receptor-positive (ER-positive) breast cancer, a drug called tamoxifen or, after menopause, drugs called aromatase inhibitors (AIs) may be suggested to lower the chance of cancer returning.
- For women who have never had breast cancer but have had an “atypical biopsy” or are at higher risk for breast cancer, tamoxifen may be suggested to lower the chance of cancer growing. For women who cannot tolerate tamoxifen, raloxifene may be suggested to lower the chance of getting breast cancer.
- These drugs lower the chance that cancer will grow or return by blocking estrogen (a hormone that can stimulate the growth of some cancers). Blocking estrogen can also lower breast density. Tamoxifen and AIs have been shown to lower breast density but raloxifene has not. Not all women taking these drugs will experience lower breast density.
Talk to your healthcare professional to decide what is right for you.
Learn More:
30. Can I change my breast density with diet or exercise? Is my breast density related to the fat in my diet?
Fat content in what you eat and exercise do not directly change breast density. But if you lose or gain a lot of weight, your breasts can look more or less dense on your mammogram – though the amount of dense tissue will stay the same. This is because if you gain weight, there will be more fatty tissue (non-dense) in your breasts. If you lose weight, you will lose fatty tissue from your breasts. So, although the foods you eat and exercising do not change your breast density, your overall body fat can affect your breast density.
While exercise does not decrease the actual amount of dense tissue in your breasts, regular physical activity does decrease the overall risk of developing breast cancer.
For more information, see Q+A #12, “Will my breasts always be dense?”.
Learn More:
31. Does taking estrogen increase breast density or breast cancer risk?
It is unclear whether taking oral (pill) or transdermal (skin patch) estrogen alone increases breast density or breast cancer risk.
Vaginal estrogen:
- Has not been shown to increase breast cancer risk in women who have not had breast cancer.
- One study found an increased risk of breast cancer recurrence in breast cancer survivors who have taken an aromatase inhibitor.
- Does not increase the risk of breast cancer death in breast cancer survivors.
- There are not many studies on vaginal estrogen and breast density.
Learn More:
32. Does taking hormone replacement therapy (HRT) treatment (combined estrogen and progesterone) increase breast density or breast cancer risk?
Yes. Increases in both breast density and breast cancer risk have been shown in patients taking estrogen and progesterone HRT. This is true in patients using oral (pill) or transdermal (skin patch) HRT.
33. If I am a breast cancer survivor, does having dense breasts increase the chance of getting cancer in my opposite breast?
Yes. If you have dense breasts and have had breast cancer, there is a greater chance of developing cancer in the opposite breast (known as contralateral breast cancer). The good news is that this risk can be reduced with medications. Please see Q+A #32, “Can I lower my breast density?”.
Learn More:
References
1. Raghavendra A, Sinha AK, Le-Petross HT, et al. Mammographic breast density is associated with the development of contralateral breast cancer. Cancer 2017; 123:1935-1940
2. Sandberg ME, Li J, Hall P, et al. Change of mammographic density predicts the risk of contralateral breast cancer–a case-control study. Breast Cancer Res 2013; 15:R57
3. Engmann NJ, Scott CG, Jensen MR, et al. Longitudinal changes in volumetric breast density with Tamoxifen and aromatase inhibitors. Cancer Epidemiol Biomarkers Prev 2017; 26:930-937
4. Cuzick J, Warwick J, Pinney E, et al. Tamoxifen-induced reduction in mammographic density and breast cancer risk reduction: a nested case-control study. J Natl Cancer Inst 2011; 103:744-752
34. Are lumpy or fibrocystic breasts the same thing as dense breasts?
No. Having “lumpy” or fibrocystic breasts is different than having dense breasts, but some women have both.
Normal breast tissue can feel lumpy whether it is fatty or dense. Cysts are common and noncancerous and sometimes are large enough to be noticed as a lump. Having dense breasts has nothing to do with the way your breasts look or feel. The doctor who reviews your mammogram determines whether you have dense breasts after looking closely at images from your mammogram.
Learn More:
35. Do men have dense breasts?
No. Normal male breasts do not contain dense tissue.
Sometimes men’s breasts do grow and look more like female breasts (known as gynecomastia). This can happen as men age or can be caused by some medicines.
It is important to remember that men can also get breast cancer. A mammogram can be done in men to check a lump.
Learn More:
36. Is breast density inherited?
If your mother or sister has dense breast tissue, it’s more likely you will too.
Learn More:
37. Do Black women have denser breasts? Do Asian women have denser breasts? Do Hispanic women have denser breasts?
Many studies have found that Asian women more often have dense breasts than women of other races. Studies differ on whether Black or Hispanic women have denser breasts than non-Hispanic white women.
What matters most is your individual breast density. If you have dense breasts, you are more likely to get breast cancer and it is more likely to be missed on the mammogram.
Learn More:
38. What if I have dense breasts and a disease-causing BRCA gene variant (mutation)?
BRCA gene mutations and dense breasts both increase the chances that a woman will get breast cancer. However, BRCA1 or BRCA2 mutations put women at a much higher risk for getting breast cancer than the risk from having dense breasts.
Because BRCA gene carriers are more likely to get breast cancer at a younger age, they usually get a breast MRI as part of their breast screening. In these women, breast screening should also start earlier, with MRI beginning at age 25 and mammography starting at age 30 or later.
MRI screening for women with BRCA mutations is suggested whether or not they have dense breasts.
Learn More: